Cancer researchers at the University of Leicester have developed a breakthrough technique that could significantly improve the way we predict how breast cancer patients respond to chemotherapy and antibody-directed cancer treatments. This new method, based on the patient-derived explant (PDE) technique, has the potential to offer more personalized treatment plans, ultimately helping doctors provide more effective therapies while avoiding unnecessary treatments that might be ineffective.
The results of this promising study were published in Scientific Reports, a peer-reviewed journal, and highlight a novel approach to cancer treatment prediction. Breast cancer remains one of the most common cancers worldwide, with 2.3 million new cases diagnosed annually. Despite advancements in early detection and treatments, it continues to be a leading cause of death among women, with around 670,000 women succumbing to the disease each year, according to the World Health Organization (WHO) data from 2022.
Although there have been remarkable strides in developing targeted therapies for specific types of breast cancer, certain tumors remain resistant to treatment. This presents a major challenge, as some patients undergo harsh treatments that, unfortunately, do not yield positive results. One of the key hurdles in cancer treatment has been understanding and predicting which therapies will be effective for a given patient’s tumor. Without accurate prediction tools, doctors are often left to rely on trial and error, resulting in unnecessary treatment courses that could cause harmful side effects and extend the suffering of the patient.
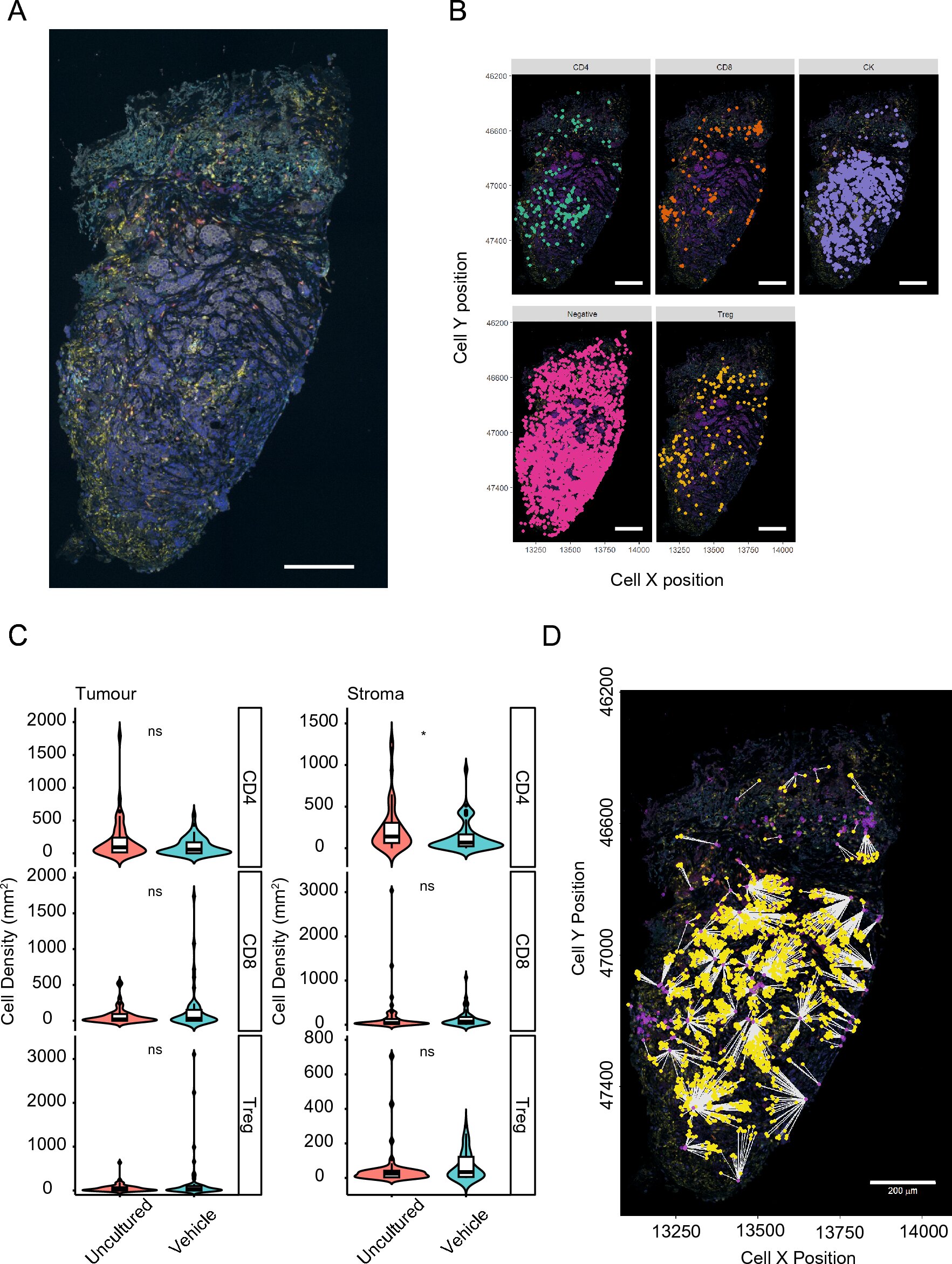
In an effort to address this problem, researchers at the University of Leicester employed advanced digital pathology and multi-immunofluorescent techniques to study breast cancer tumor samples in a controlled laboratory environment. These cutting-edge technologies allowed them to observe and measure the stability of patient-derived tumor explants over time, offering valuable insights into the tumor’s behavior and response to treatment before actual clinical treatment takes place.
Gareth Miles, a lecturer in Cancer Patient Derived Explant Technology at the University of Leicester, explained that in the era of personalized medicine, targeted therapies for different types of breast cancer are now available. However, there remains a subset of tumors that are particularly challenging to treat. Historically, it has been difficult to predict how well a patient’s tumor will respond to a specific treatment. This uncertainty often leads to patients enduring treatments that do not work, causing unnecessary harm.
Miles stressed that developing a more accurate and reliable method of predicting treatment outcomes in the lab could substantially improve clinical outcomes. By testing the effectiveness of different therapies on patient tumor samples before administering them to the patient, doctors can better tailor their treatment strategies and avoid the frustration of ineffective therapies. This would ultimately help save time, reduce patient suffering, and improve survival rates.
This latest study builds on previous research by the same team, where they had applied the PDE technique to study non-small cell lung cancer and endometrial cancer. Their earlier findings showed a significant relationship between how patient-derived explants responded to chemotherapy drugs in the lab and the actual clinical outcomes of the patients. This encouraging discovery laid the groundwork for the team’s work on breast cancer, where they focused on observing the behavior of tumor explants from 55 breast cancer patients.
The research team subjected these breast cancer tumor explants to treatment with either chemotherapy or HER2 antibody therapy trastuzumab in a laboratory setting. The researchers then monitored the explants’ responses to these treatments and compared the results with the actual clinical progression of the patients. Remarkably, the team found that the tumors in the lab responded to treatment in a similar way to how they had responded in the patients themselves, validating the potential of this PDE method as a predictive tool for clinical treatment.
Professor Catrin Pritchard, Professor of Cancer Biochemistry at the University of Leicester, added that one of the most encouraging aspects of their findings was the preservation of the tumor’s architecture and immune microenvironment throughout the testing process. The team’s technique allowed the tumor explants to maintain their structure for up to 72 hours during the experiment, which is a significant achievement. Previous methods had struggled to preserve the integrity of the tumor during such prolonged testing, but this new technique ensures that the lab results accurately reflect the behavior of the tumor in the patient.
This breakthrough holds great promise in clinical oncology. By using this technique, doctors can more accurately predict how individual tumors will react to specific therapies, helping them make informed decisions about which treatment options to pursue. Rather than subjecting patients to ineffective therapies, doctors can identify the most promising treatments from the outset, improving the likelihood of success and enhancing the overall quality of care.
The research team’s findings suggest that their PDE method could serve as a valuable preclinical testing platform for breast cancer patients. If widely adopted, it could reduce the reliance on trial-and-error treatment approaches, ultimately helping to speed up the development of personalized treatment plans. With more targeted therapies, patients are likely to experience fewer side effects and improved outcomes.
This study also reinforces the importance of precision medicine in cancer treatment. By harnessing the power of advanced technologies and innovative techniques like the PDE method, doctors can move closer to providing truly personalized care for cancer patients, addressing the unique characteristics of each individual’s disease. The ability to predict treatment responses with greater accuracy could be a game changer in the fight against breast cancer and other cancers that remain difficult to treat.
Reference: Constantinos Demetriou et al, An optimised patient-derived explant platform for breast cancer reflects clinical responses to chemotherapy and antibody-directed therapy, Scientific Reports (2024). DOI: 10.1038/s41598-024-63170-0
Think this is important? Spread the knowledge! Share now.