A groundbreaking predictive tool developed by researchers at the Florey Institute of Neuroscience and Mental Health, in collaboration with the Alzheimer’s Disease Neuroimaging Initiative (ADNI) and the Australian Imaging, Biomarker, and Lifestyle (AIBL) study, promises to revolutionize how clinicians and patients plan for the onset of mild cognitive impairment (MCI) and Alzheimer’s disease (AD). This tool, known as the Florey Dementia Index (FDI), can accurately predict the age at which an individual might develop MCI or AD, with an impressive level of precision that could transform the way we approach early diagnosis and treatment. The FDI has shown the ability to predict the onset of MCI within an average of 2.78 years and AD onset within 1.48 years, offering a significant breakthrough in predictive neurodegenerative disease science.
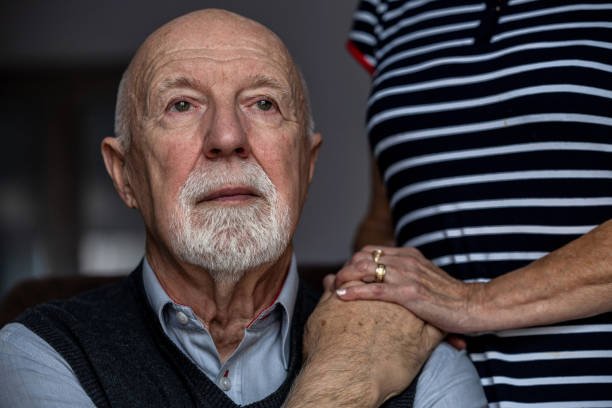
Alzheimer’s disease, a progressive neurodegenerative disorder, is characterized by a gradual decline in cognitive function, which starts with MCI before eventually developing into dementia. The transition from MCI to full-blown dementia is particularly challenging, as it significantly impacts an individual’s ability to function independently. For years, scientists have been searching for a reliable clinical tool that could predict the age at which this transition from MCI to AD would occur, and the FDI appears to be the solution that could help answer this longstanding question.
Previous research has suggested early indicators of Alzheimer’s disease, such as changes in the gut microbiome, but clinical tools for predicting the onset age of AD have remained elusive. The absence of such a tool has made it difficult for clinicians to provide early intervention and care before the presentation of classic symptoms. However, with the advent of the Florey Dementia Index, patients and clinicians may now be able to predict with greater accuracy when the onset of MCI or AD will occur, allowing for earlier care planning and the prioritization of treatments before significant cognitive decline begins.
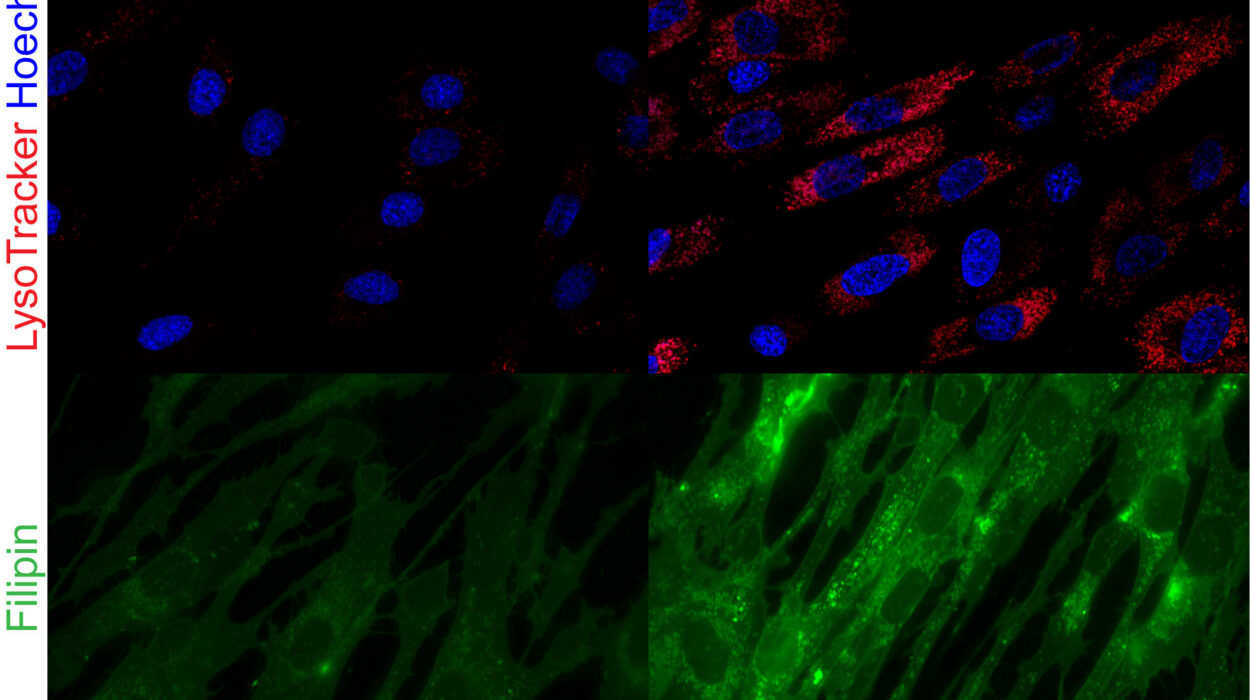
Developed through a robust statistical modeling approach, the FDI leverages a combination of noninvasive data points to offer predictions. The tool uses two key inputs: age and Clinical Dementia Rating Sum of Boxes (CDR-SB) scores. These data points are gathered through widely accessible, noninvasive methods, providing an ideal balance between accuracy and feasibility. The tool’s noninvasive nature means that it can be easily integrated into routine clinical practice, ensuring that clinicians can utilize it in a practical and cost-effective manner.
The FDI was tested using data from 3,694 participants drawn from both the AIBL and ADNI cohorts, spanning nearly two decades of research from October 2004 to March 2023. In addition, the tool’s applicability was tested using data from the Anti-Amyloid Treatment in Asymptomatic Alzheimer’s (A4) study, which involved 93 participants. These participants were part of a simulated trial designed to evaluate the FDI’s performance in a cohort with preclinical Alzheimer’s disease, a stage prior to the onset of MCI. The study’s results confirmed the predictive power of the FDI, demonstrating its ability to forecast MCI and AD onset with considerable accuracy.
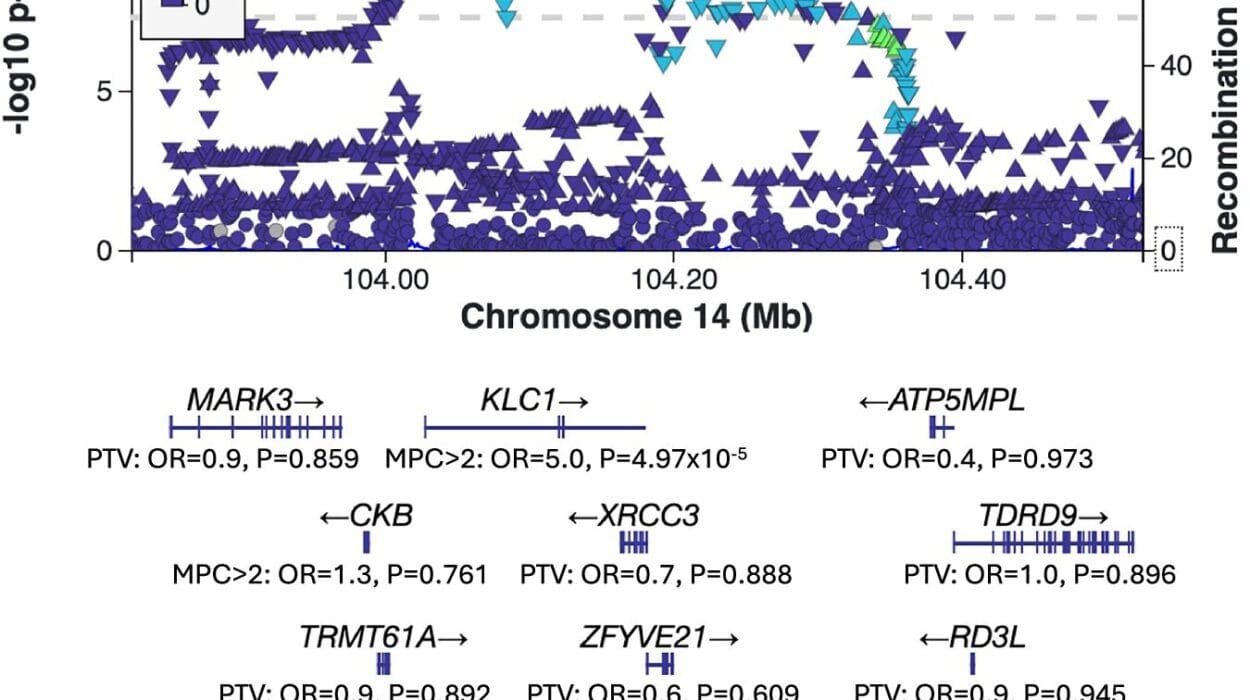
Among the participants from AIBL and ADNI, the FDI accurately predicted the onset of MCI and AD, with a mean absolute error (MAE) of 2.78 years for MCI onset and 1.48 years for AD onset. These figures represent a significant achievement in terms of prediction accuracy, as they show that the FDI can predict disease onset with minimal error. In the A4 trial, which focused on preclinical Alzheimer’s disease, the tool performed even better, with MAEs of just 1.57 years for MCI onset and an impressive 0.70 years for AD onset. These results suggest that the FDI could be especially useful for identifying individuals who are at risk of developing AD in its earliest stages.
What makes the FDI particularly remarkable is its robustness and generalizability across different datasets. The researchers did not make any adjustments for comorbidities or demographic factors such as sex when initially testing the model, yet the FDI consistently demonstrated high levels of accuracy. This is a key feature that makes the tool so promising, as it suggests that the model could be used universally, regardless of a patient’s specific medical history or background. However, when the study did incorporate common comorbidities, such as hypertension, stroke, and psychiatric disorders, into the model, the FDI’s performance improved slightly, further reinforcing its versatility.
Incorporating demographic factors such as sex into the FDI model also led to a small improvement in the model’s performance for predicting AD onset, though it had no significant effect on predicting MCI onset. This suggests that while the FDI is robust in general, it may be possible to enhance its predictive capabilities further by fine-tuning it with additional personalized factors, particularly for individuals at higher risk of developing AD.
One of the more intriguing findings of the study was the survival analysis, which revealed specific thresholds in the FDI scores that were associated with a rapid decline in dementia-free probability. According to the study, an FDI threshold of 79 was closely linked to the onset of MCI, while an FDI score of 85 was strongly associated with the onset of AD. These thresholds could offer clinicians actionable markers that signal when patients should begin considering more intensive diagnostic tests or intervention strategies.
The potential clinical applications of the FDI are vast. By providing clinicians with an accessible and accurate tool for predicting the onset of MCI and AD, the FDI could allow for better long-term care planning. This might include early interventions that are crucial in slowing disease progression, improving quality of life, and helping patients retain independence for as long as possible. The ability to predict the onset of MCI and AD could also help prioritize patients for treatment with emerging disease-modifying therapies, such as monoclonal antibody drugs that target the underlying biological mechanisms of Alzheimer’s disease.
For patients and their families, the FDI could offer invaluable insight into the future course of the disease, allowing them to make informed decisions about long-term care, legal planning, and lifestyle changes while they are still capable of doing so. Early knowledge of disease onset would also give families more time to adapt and plan for the challenges associated with dementia and home care, ensuring that patients receive the support they need at the right time.
Despite the promising results, the study acknowledges that further validation is necessary before the FDI can be fully integrated into clinical practice. Testing the tool in larger and more diverse cohorts will be crucial for assessing its applicability across different populations. In addition, while the FDI has shown impressive results in predicting the onset of MCI and AD, it remains essential to consider other factors, such as genetic risk factors, environmental influences, and individual health histories, to create a truly comprehensive approach to dementia care.
Nevertheless, the Florey Dementia Index marks a significant step forward in personalized dementia care. With its ability to predict disease onset with high accuracy and its reliance on noninvasive, widely accessible data, the FDI offers a powerful new tool for clinicians, patients, and families alike. As research into Alzheimer’s disease continues to evolve, the FDI could play a central role in transforming how we approach early detection, intervention, and treatment, ultimately improving the lives of millions of individuals affected by neurodegenerative diseases like Alzheimer’s.
Reference: Chenyin Chu et al, Development and Validation of a Tool to Predict Onset of Mild Cognitive Impairment and Alzheimer Dementia, JAMA Network Open (2025). DOI: 10.1001/jamanetworkopen.2024.53756