Recent research published in the European Heart Journal has unveiled a potentially alarming link between pockets of fat hidden within muscles—referred to as intermuscular fat—and an increased risk of heart disease, heart failure, and death, independent of traditional health metrics such as body mass index (BMI). The study, the first of its kind to thoroughly investigate the impact of intermuscular fat on cardiovascular health, reveals that individuals with greater quantities of this fat face an elevated risk of adverse heart outcomes. This finding signals a shift in how we assess and evaluate cardiovascular health, emphasizing the limitations of conventional methods like BMI and waist circumference.
The Role of Intermuscular Fat in Heart Disease
Intermuscular fat is a type of body fat that is stored between muscles, unlike the fat found directly beneath the skin (subcutaneous fat) or around vital organs (visceral fat). In beef, it is the marbling fat that enhances the flavor and tenderness of steaks, but in humans, it may be far less desirable for overall health. While previous studies have primarily focused on the well-known risks associated with obesity and visceral fat, little research has been conducted on intermuscular fat and its impact on cardiovascular health. The recent study conducted by Professor Viviany Taqueti and her team at Brigham and Women’s Hospital in Boston sought to fill this gap by analyzing the influence of fat stored within muscles on heart disease.
This groundbreaking study showed that high levels of intermuscular fat could significantly elevate the risk of coronary microvascular dysfunction (CMD)—a condition where the small blood vessels of the heart become impaired. The consequences of this dysfunction can be severe, leading to increased susceptibility to heart failure, heart attacks, and in some cases, death.
Study Overview and Methodology
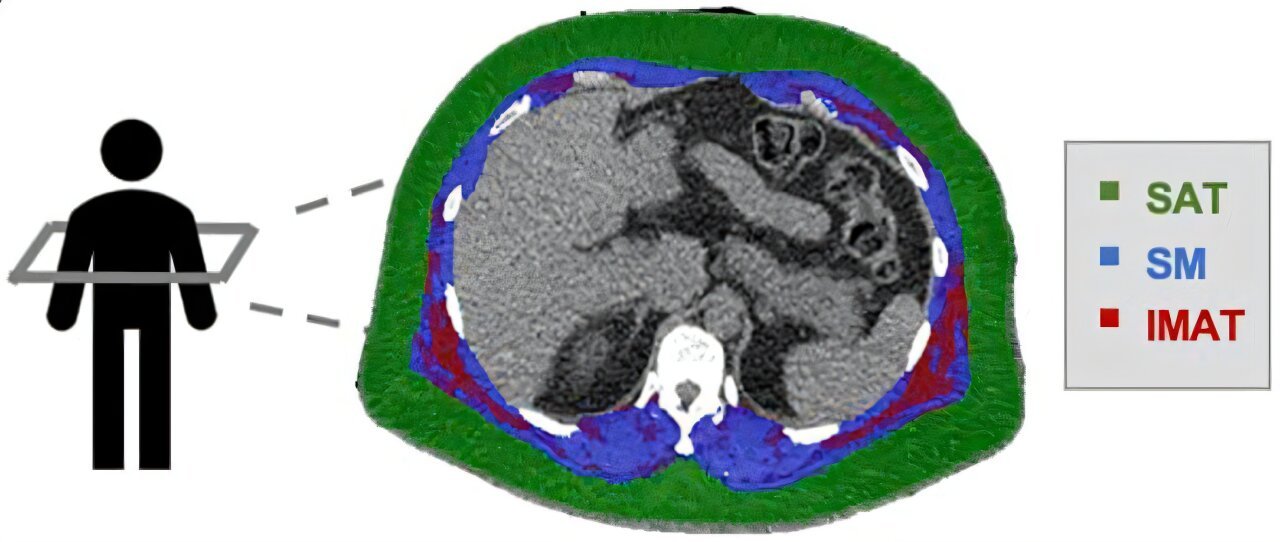
The study involved 669 patients who were being evaluated at Brigham and Women’s Hospital for symptoms such as chest pain and shortness of breath, but who had no obstructive coronary artery disease (no blocked arteries). These patients, averaging 63 years of age, were predominantly female (70%) and nearly half were non-white (46%). The researchers utilized a combination of advanced imaging techniques—cardiac positron emission tomography (PET) scans and computed tomography (CT) scans—to assess heart function and examine body composition. Through these scans, the amount and distribution of fat and muscle in each patient’s torso were quantified.
To understand the role of intermuscular fat, researchers introduced a new metric called the “fatty muscle fraction.” This ratio compared the amount of fat stored in the muscles to the total volume of muscle and fat in a given region. Following up with the patients over a period of approximately six years, researchers tracked whether the patients experienced any hospitalizations, heart attacks, heart failure, or death.
Findings and Implications
The results from the study were revealing and concerning. Individuals with higher levels of intermuscular fat were at a greater risk of developing CMD and subsequent serious heart conditions. For every 1% increase in fatty muscle fraction, the risk of CMD rose by 2%, and the risk of heart disease-related complications increased by a significant 7%. These associations remained even after accounting for other established cardiovascular risk factors, including BMI, age, and gender. Notably, people with both high levels of intermuscular fat and evidence of CMD had the highest risk of experiencing heart attack, heart failure, and death.
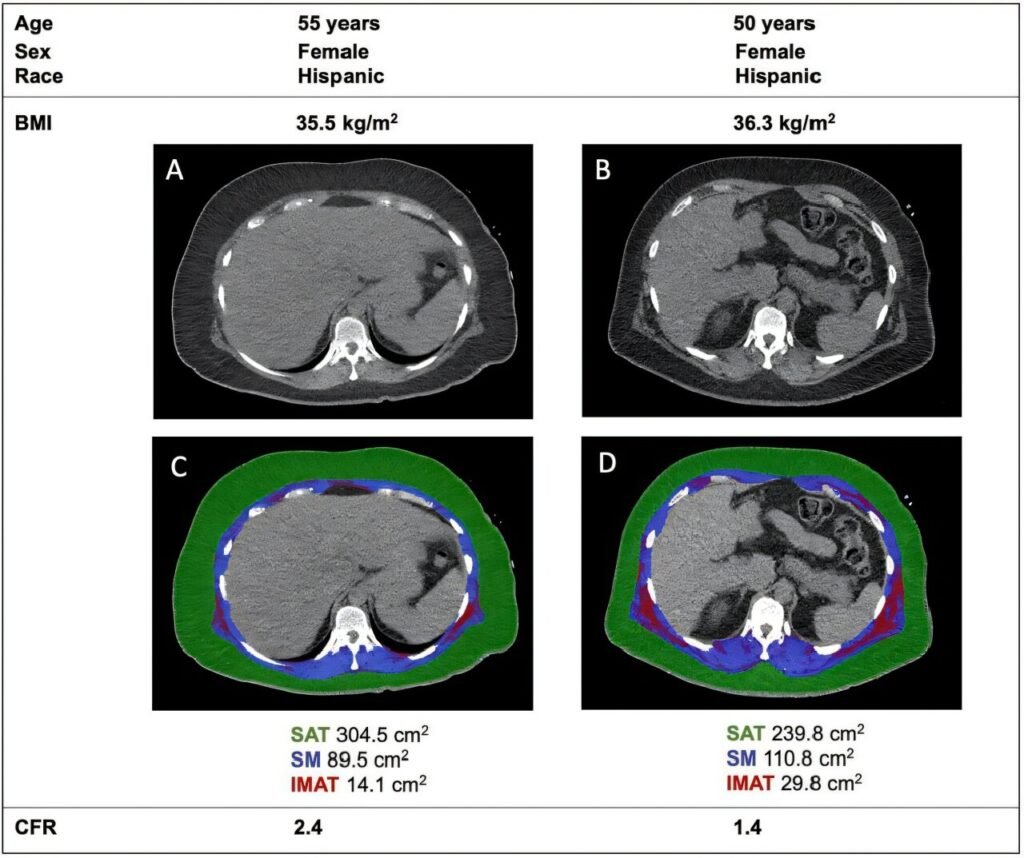
Interestingly, the researchers observed that lean muscle mass seemed to offer a protective effect against cardiovascular issues. Those with a higher proportion of lean muscle were at a reduced risk of adverse cardiovascular outcomes, even when they carried excess fat elsewhere in the body. On the other hand, fat stored under the skin (subcutaneous fat), which has been a focus of previous research, was not linked to an increased risk of heart disease.
The Potential Mechanisms Behind Intermuscular Fat and Heart Disease
Professor Taqueti hypothesized that intermuscular fat may contribute to inflammation, altered glucose metabolism, and insulin resistance, all of which are known to exacerbate heart disease. She explained that fat stored in muscles could provoke low-grade inflammation, which, over time, damages blood vessels, including those supplying the heart. This chronic inflammation could lead to further health problems, such as metabolic syndrome, which is a cluster of conditions—like high blood pressure, high cholesterol, and obesity—that significantly increases the risk of heart disease.
The presence of intermuscular fat may also disrupt the balance of fat-burning and fat-storing processes in the body. This could lead to negative impacts on metabolic function, impairing the body’s ability to use energy efficiently and increasing the likelihood of heart complications.
The Limitations of Body Mass Index (BMI)
This research underscores a critical flaw in the current methods of assessing cardiovascular risk. BMI has long been a standard metric for determining obesity levels, but it has increasingly come under scrutiny for its limitations. BMI does not differentiate between lean muscle mass and fat, nor does it account for where fat is stored in the body. Consequently, BMI alone may not provide a complete or accurate picture of an individual’s risk for heart disease.
The study’s findings suggest that people with similar BMIs may have very different body compositions and, therefore, very different risks for cardiovascular disease. For example, a person with a BMI in the “overweight” or “obese” range, but who has more lean muscle and less intermuscular fat, may have a lower risk of heart disease than someone with a BMI in the same range, but with higher amounts of intermuscular fat.
Professor Taqueti emphasized that intermuscular fat could be a key factor in identifying individuals at high risk for heart disease—an advancement that would provide additional precision in cardiovascular risk assessments. “Knowing that intermuscular fat raises the risk of heart disease gives us another way to identify people who are at high risk, regardless of their body mass index,” she stated.
The Future of Cardiovascular Health Research and Treatment
While the findings of this study are important, much remains unknown about how to mitigate the risks associated with intermuscular fat. Although the study suggests that fat in muscles has a direct influence on cardiovascular health, it is unclear how lifestyle interventions, such as exercise, dietary changes, or medications, might specifically target and reduce fat stored in muscles.
Some of the next steps in research will involve assessing how different treatment approaches, such as weight-loss drugs, exercise routines, or nutritional interventions, might affect the fat composition within muscles and the associated risks. For example, the new class of glucagon-like peptide-1 (GLP-1) receptor agonists, which are used to treat type 2 diabetes and obesity, could play a role in reducing intermuscular fat and lowering the cardiovascular risk.
The research team is also exploring the relationship between other factors, like muscle quality, skeletal muscle physiology, and exercise capacity, and how these aspects might influence heart disease outcomes.
Broader Implications for Cardiovascular Health
An accompanying editorial by Dr. Ranil de Silva, a researcher at Imperial College London, highlights the broader implications of the study’s findings. He acknowledges the complexity of the relationship between obesity and cardiovascular risk, noting that while obesity has long been associated with heart disease, the impact of specific types of fat remains poorly understood. The identification of intermuscular adipose tissue (IMAT) as a key player in CMD and heart disease could pave the way for more refined and individualized strategies for managing heart health.
The study’s findings may also have profound implications for how we approach cardiovascular disease prevention, diagnosis, and treatment. Instead of focusing solely on BMI and waist circumference as indicators of heart disease risk, future clinical guidelines could incorporate assessments of intermuscular fat. Early identification of individuals with higher fatty muscle fractions could prompt earlier interventions, such as personalized weight management plans, targeted treatments, and tailored exercise regimens.
Conclusion
The research led by Professor Viviany Taqueti and her colleagues offers important new insights into the role of intermuscular fat in cardiovascular health, adding an important layer to our understanding of how body composition affects heart disease risk. As the research community delves deeper into the mechanisms behind these findings, we may develop better tools to evaluate cardiovascular risk and more effective ways to combat the heart disease epidemic. For now, however, this study reinforces the need for a more nuanced approach to understanding obesity and cardiovascular health—one that considers the type, location, and amount of fat in the body, rather than relying solely on metrics like body mass index.
Reference: Viviany R. Taqueti et al, Skeletal Muscle Adiposity, Coronary Microvascular Dysfunction, and Adverse Cardiovascular Outcomes, European Heart Journal (2024). DOI: 10.1093/eurheartj/ehae827
Think this is important? Spread the knowledge! Share now.