CAR T cell therapy has emerged as one of the most promising new cancer treatments in recent years, offering hope for patients battling certain types of cancer, particularly those with blood cancers like leukemia and lymphoma. This cutting-edge treatment involves modifying a patient’s own T cells, a type of white blood cell, to target and attack cancer cells more effectively. While CAR T cell therapy has shown remarkable success, a major limitation has been the need for patients to wait for their own T cells to be collected, engineered, and reintroduced into their body—a process that can take weeks, sometimes at the cost of precious time.
However, groundbreaking research from Memorial Sloan Kettering Cancer Center (MSK) has introduced a potential game-changing solution that could transform the field of CAR T cell therapy. This new advance could enable the use of off-the-shelf CAR T cells, sourced from healthy donors and stored for immediate use in cancer patients, eliminating the need for time-consuming customization of cells. This development, described in a Nature study, holds significant promise for making CAR T cell therapy more accessible, efficient, and affordable, potentially saving lives by providing a faster, more reliable cancer treatment.
The Challenge with Autologous CAR T Cell Therapy
The traditional method of autologous CAR T cell therapy involves extracting T cells from a patient’s own blood, then genetically modifying these cells in the laboratory to express receptors that allow them to recognize and destroy cancer cells. Once the cells are engineered, they are infused back into the patient’s bloodstream, where they target the cancer. While this approach has been effective for many patients, it comes with several challenges:
- Time delay: The process of collecting and modifying a patient’s own T cells can take several weeks, and in cases where a patient is in urgent need of treatment, this delay could be fatal.
- Personalization: Every patient’s T cells are unique, so each treatment must be customized for the individual, requiring significant resources and time.
Despite the remarkable success of CAR T cell therapy, especially in the treatment of certain cancers like B-cell lymphomas and acute lymphoblastic leukemia (ALL), the need for a quicker and more widely accessible solution remains pressing.
The Promise of Allogeneic CAR T Cells
Researchers at MSK have now developed a way to address this limitation by utilizing allogeneic CAR T cells—T cells from healthy donors rather than from the patient. These cells can be stored in advance and made readily available for infusion into cancer patients. However, using donor cells presents a significant challenge: the immune system of the patient may recognize the donor cells as foreign, leading to rejection or other immune responses, including graft-versus-host disease (GVHD), in which the donor T cells attack the recipient’s tissues.
To overcome these obstacles, the researchers at MSK have pioneered an innovative approach that modifies the allogeneic CAR T cells to prevent immune rejection and ensure that they persist in fighting cancer. This method could ultimately allow for off-the-shelf CAR T cell therapies that do not require the patient to undergo the lengthy process of harvesting and engineering their own cells.
The Breakthrough: Nef and Immune Evasion
The key discovery in this research centers around a protein called Nef, which is used by the HIV virus to evade detection and destruction by the immune system. This protein provides a powerful mechanism for protecting the virus from immune attack, allowing it to survive and replicate within the host’s cells. Researchers wondered if Nef could similarly help donor CAR T cells evade immune detection when transplanted into a cancer patient.
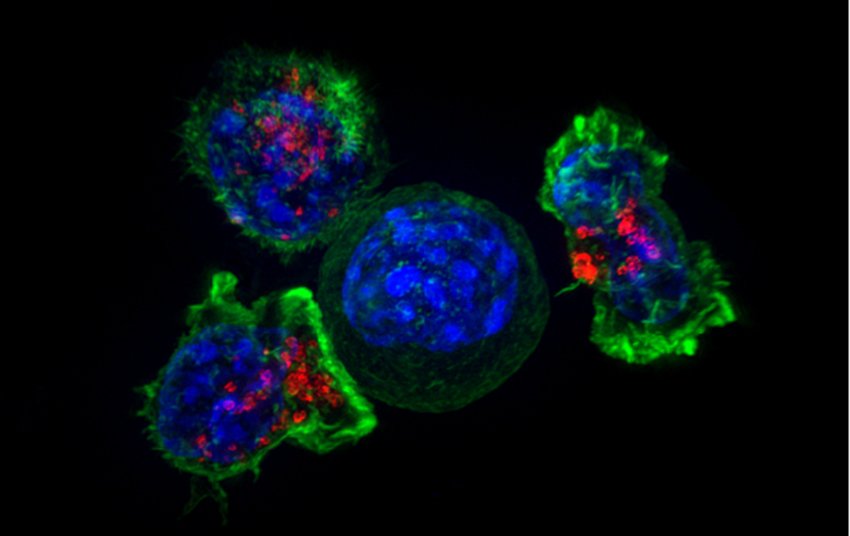
Using advanced genetic techniques, including the CRISPR gene-editing tool, the team inserted the Nef protein into donor-derived CAR T cells. The results were promising: the modified CAR T cells were able to survive and persist in a mouse model of cancer for an extended period, showing both effective immune evasion and sustained cancer-fighting activity.
Dr. Karlo Perica, the study’s first author and a physician-scientist at MSK, explained the dual benefits of Nef in these cells: first, it reduces HLA-I expression on the surface of the CAR T cells. HLA-I molecules are typically recognized by the immune system as “self” or “non-self,” and their presence can trigger an immune response if the cell is seen as foreign. By reducing this signal, Nef helps the CAR T cells remain undetected by the patient’s immune system. Second, Nef protects the CAR T cells from a process called apoptosis—the programmed cell death that normally eliminates damaged or unnecessary cells. Together, these mechanisms allow the engineered cells to survive longer and remain potent in fighting the cancer.
Implications for Faster, Safer Treatment
This research represents a significant leap forward for the development of allogeneic CAR T cell therapies. If this approach proves effective in clinical trials, it could drastically reduce the waiting time for cancer patients who need CAR T cell therapy, making it possible to deliver life-saving treatment more quickly. By using pre-made, donor-derived cells, medical centers would be able to provide a ready-to-use product for patients in need, bypassing the lengthy process of harvesting and modifying the patient’s own cells.
Currently, allogeneic CAR T cells are being tested for multiple myeloma, a type of blood cancer. In these trials, patients receive immune-suppressing drugs to prevent rejection of the donor cells. However, the new findings from MSK could lead to the development of allogeneic CAR T cells that do not require immune suppression, reducing the risks of infections and other side effects that come with immunosuppressive therapies.
The use of donor-derived CAR T cells could also offer an advantage in terms of cell quality. Many cancer patients, particularly those who have undergone extensive chemotherapy, may have weakened immune systems that produce suboptimal T cells. By contrast, donor T cells from healthy individuals are more likely to be robust and capable of fighting cancer, increasing the likelihood of treatment success.
Expanding Access to Life-Saving Treatment
The ability to use off-the-shelf CAR T cells has the potential to greatly expand access to this life-saving therapy, making it more widely available to patients who may not otherwise have access to customized treatments. Moreover, it could significantly reduce the costs of CAR T cell therapies, making them more affordable for healthcare systems and patients alike. The overall cost of manufacturing personalized CAR T cells remains high, and reducing the reliance on individualized processes could help drive down costs, potentially enabling wider use of the treatment for various types of cancer.
Dr. Michel Sadelain, a pioneer in CAR T cell therapy and the principal investigator of the study, emphasized the importance of these findings in the broader context of cancer treatment. He noted that off-the-shelf CAR T cells would remove the need for manufacturing personalized therapies, ultimately making this treatment more scalable and available to a larger number of patients.
Moving Toward Clinical Trials
While the study’s findings are still in the preclinical stage, the researchers are optimistic that they will be able to move toward clinical trials in the near future. If these off-the-shelf CAR T cells prove effective in human patients, they could mark a transformative step in the fight against cancer, offering a faster, more reliable treatment option for those in urgent need.
As Dr. Perica puts it, “The multiple discoveries coming out of Dr. Sadelain’s lab have helped bring us closer to the day when we have CAR T cells right at hand to give to patients without delay.”
Conclusion
The development of off-the-shelf allogeneic CAR T cells represents a monumental advancement in the fight against cancer. By engineering donor-derived CAR T cells that can evade immune rejection and persist in the body, researchers at MSK have opened the door to a future where cancer patients no longer have to wait for weeks for personalized treatments. This breakthrough could not only improve the effectiveness and availability of CAR T cell therapy but also make it more accessible and affordable, potentially transforming cancer care for a wide range of patients. As clinical trials progress, the hope is that this new approach will bring the benefits of CAR T cell therapy to even more patients, offering a lifeline to those battling cancer.
Reference: Karlo Perica et al, HIV immune evasin Nef enhances allogeneic CAR T cell potency, Nature (2025). DOI: 10.1038/s41586-025-08657-0