In a groundbreaking development for cancer genetics, a multi-institutional, international study led by researchers from the Mayo Clinic Comprehensive Cancer Center has provided significant insights into genetic alterations in the BRCA2 gene, an essential player in hereditary cancer risk. The study’s findings promise to revolutionize the way genetic testing for cancer risk is conducted, offering greater precision in risk assessment and the potential for personalized treatment strategies. Published in the prestigious journal Nature, the study focuses on the classification of variants of uncertain significance (VUS) within the BRCA2 gene, a key factor in the genetic basis of cancer predisposition.
The BRCA2 gene, located on chromosome 13, produces a protein crucial for repairing damaged DNA and maintaining the stability of the cell’s genetic material. Mutations in this gene can impair DNA repair, leading to the accumulation of genetic errors that may increase the risk of certain cancers, notably breast, ovarian, prostate, and pancreatic cancers. Although some mutations in BRCA2 have been definitively linked to increased cancer risk, many genetic variants within the gene remain classified as VUS due to insufficient evidence about their effects. VUS have posed a major challenge in clinical genetics, leaving both patients and healthcare providers uncertain about the implications of these variants.
The Mayo Clinic-led team conducted a comprehensive functional assessment of nearly 7,000 potential variants within the DNA-binding domain of BRCA2, the region of the gene most critical for its DNA repair function. This extensive evaluation used the cutting-edge CRISPR-Cas9 gene-editing technology, which allows researchers to modify specific genes in living organisms with unprecedented accuracy. By using CRISPR-Cas9 to analyze the biological impact of these variants, the team could directly assess how each one affected the BRCA2 protein’s ability to repair DNA, thus determining whether a given variant contributed to cancer risk.
The results were striking. The team successfully classified 91% of the VUS in the BRCA2 DNA-binding domain, bringing clarity to a category of genetic variants that has long been a source of confusion in clinical genetics. This represents a dramatic improvement in the accuracy of genetic testing, as clinicians will now be able to distinguish between harmful and benign variants with far greater precision. By eliminating much of the uncertainty surrounding VUS, healthcare providers can offer more accurate cancer risk assessments, better-targeted prevention strategies, and personalized treatment plans for patients carrying these genetic variants.
“This research is a major advancement in understanding the role of many BRCA2 variants in cancer predisposition,” says Dr. Fergus Couch, a key investigator in the study and the Zbigniew and Anna M. Scheller Professor of Medical Research at Mayo Clinic. “Until now, patients who carried VUS often worried about their cancer risk, but with the classification of these variants, we can provide a clearer picture of cancer risk and tailor both prevention strategies as well as breast cancer treatment accordingly.”
The practical implications of these findings are immense. Genetic testing laboratories and healthcare professionals can now use the comprehensive catalog of classified BRCA2 variants to guide clinical care. For patients previously identified with a VUS, this study provides an opportunity for reclassification, which may result in updated genetic test reports. The results will likely impact many individuals who previously faced ambiguity about their cancer risk due to the presence of VUS. By providing a more definitive risk assessment, doctors can offer personalized guidance on cancer screening, preventive measures, and, where appropriate, treatment options.
One of the most exciting applications of these findings is in the area of targeted cancer therapies. Genetic alterations in BRCA2 are already known to make tumors more susceptible to certain therapies, such as PARP inhibitors, which block a secondary DNA repair pathway that cancer cells with defective BRCA2 rely on. As a result of the study’s comprehensive classification of BRCA2 variants, oncologists can identify patients with mutations that may benefit from these targeted therapies. For instance, women with breast cancer or ovarian cancer who carry specific BRCA2 variants might be more likely to respond to treatments like olaparib, a PARP inhibitor that has shown promise in treating cancers associated with BRCA1 and BRCA2 mutations.
“We now have a catalog of every possible VUS in this part of BRCA2 that can be used to guide clinical care,” says Dr. Couch. “This represents a powerful resource for clinicians, enabling them to make more informed decisions about how to manage patients with these genetic variants.”
In addition to its immediate clinical impact, the study lays the groundwork for future research that could expand the understanding of BRCA2 variants across different populations and cancer types. Although the current study focused on the DNA-binding domain of BRCA2, it is expected that similar efforts will be undertaken to explore the remaining regions of the gene, as well as other genes associated with hereditary cancer risk. By analyzing BRCA2 variants in a broader range of populations, including those with diverse ethnic backgrounds, the research could help refine cancer risk predictions for a wider group of individuals, further enhancing the precision of genetic testing.
Moreover, the study highlights the potential for genetic testing to evolve into a more personalized and effective tool in the fight against cancer. As genetic testing becomes more integrated into routine healthcare, the ability to classify genetic variants with greater certainty will empower individuals to make better-informed decisions about their health. Whether through earlier screenings, preventive measures like prophylactic surgeries, or the use of targeted therapies, a more precise understanding of genetic alterations will play a critical role in reducing cancer risk and improving patient outcomes.
The Mayo Clinic Comprehensive Cancer Center’s research also has implications for improving the efficiency of cancer prevention programs worldwide. Genetic testing is increasingly becoming a part of routine screening, especially for individuals with a family history of cancer. By refining the classification of genetic variants, this study ensures that patients receive more accurate counseling regarding their cancer risks. For example, a patient who previously carried a VUS in BRCA2 may now learn that their specific variant does not increase their risk, reducing unnecessary worry and allowing them to focus on other preventive health measures. Alternatively, a patient whose variant is now classified as pathogenic can be guided towards more proactive interventions, such as increased surveillance or prophylactic treatments.
Beyond its impact on individual patients, this study also strengthens the case for widespread genetic testing in cancer prevention. As the cost of genetic testing continues to fall and its availability increases, more individuals may seek testing to understand their hereditary cancer risks. By providing clear and actionable data, the findings from this study enhance the overall utility of genetic testing, making it a more effective tool for both preventive care and targeted treatment strategies.
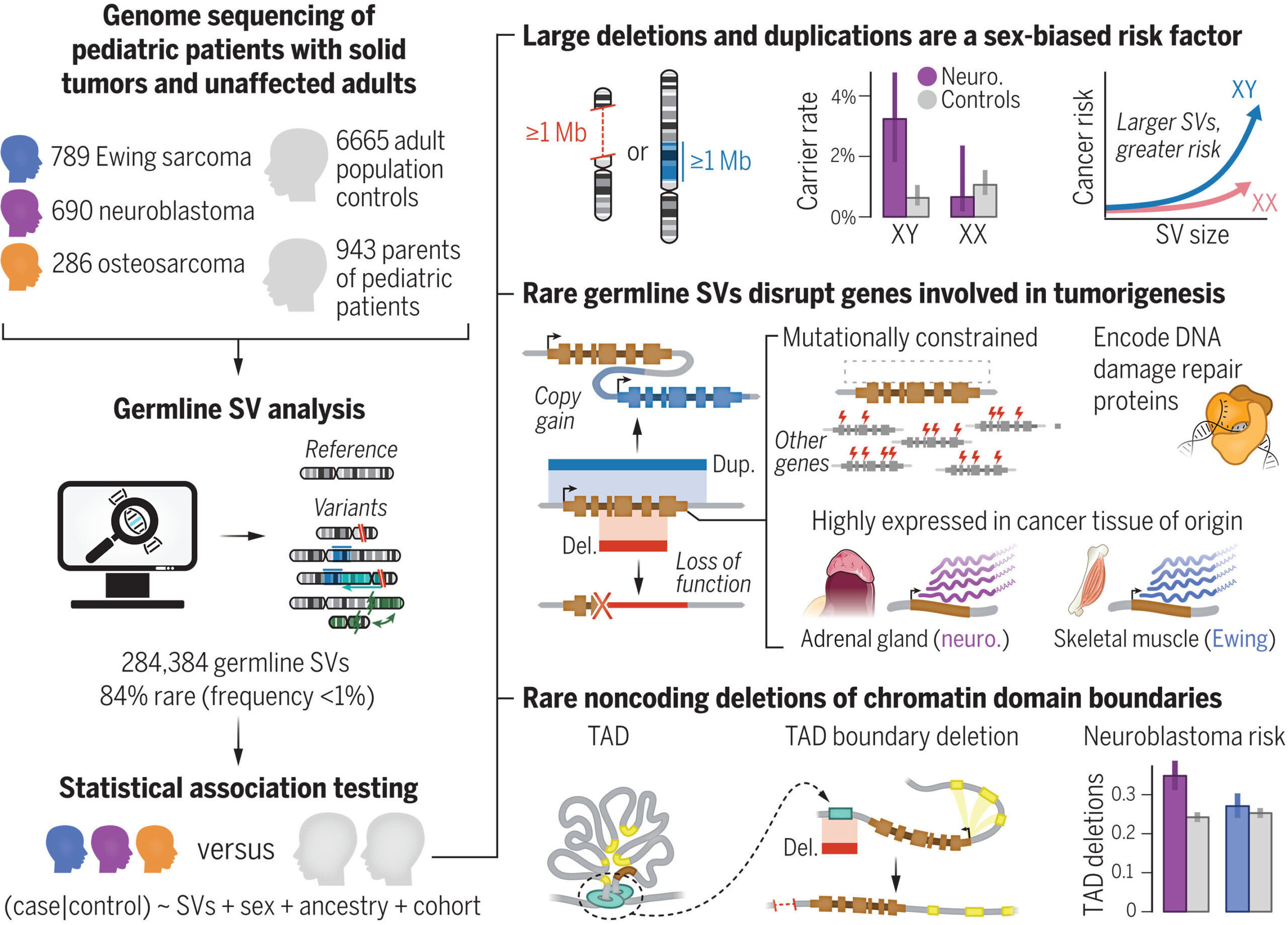
References: Riaz Gillani et al, Rare germline structural variants increase risk for pediatric solid tumors, Science (2025). DOI: 10.1126/science.adq0071
Jayne Y. Hehir-Kwa et al, Inherited genome instability, Science (2025). DOI: 10.1126/science.adu6125