Vision loss caused by retinal degeneration has long been considered irreversible. Diseases such as age-related macular degeneration (AMD) and retinitis pigmentosa lead to the progressive death of light-sensitive cells in the retina, ultimately resulting in blindness. Current treatments focus on slowing disease progression, but they do not offer a way to replace the lost cells. However, a groundbreaking study conducted by researchers at Wenzhou Medical University and collaborating institutions has identified a population of human neural retinal stem-like cells with the ability to regenerate retinal tissue and restore vision.
This discovery challenges the long-held belief that humans lack retinal stem cells capable of regeneration. Unlike fish and amphibians, which continuously generate new retinal cells from a specific stem cell population, mammals were thought to lack a similar mechanism. For over two decades, scientists have debated whether such cells might exist in the human retina, and this study provides compelling evidence that they do.
Uncovering Retinal Stem-Like Cells in Human Tissue
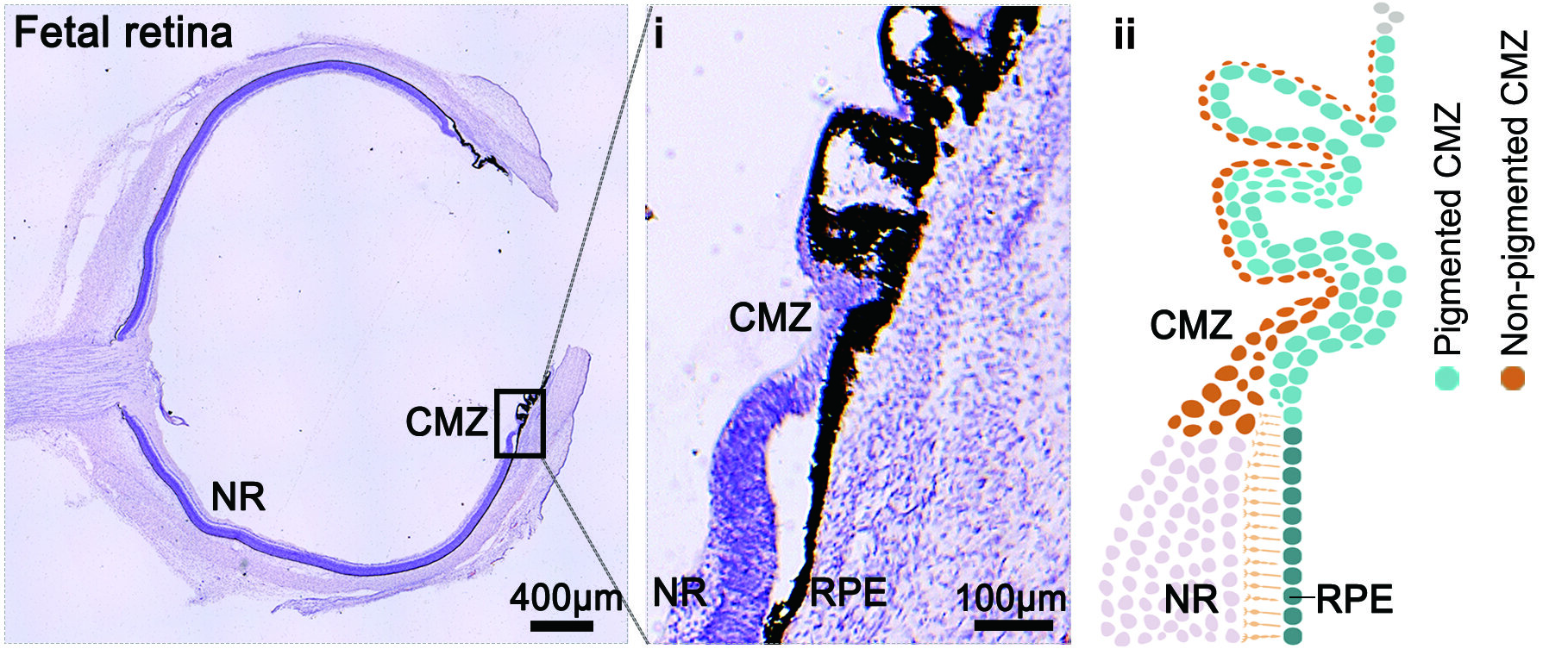
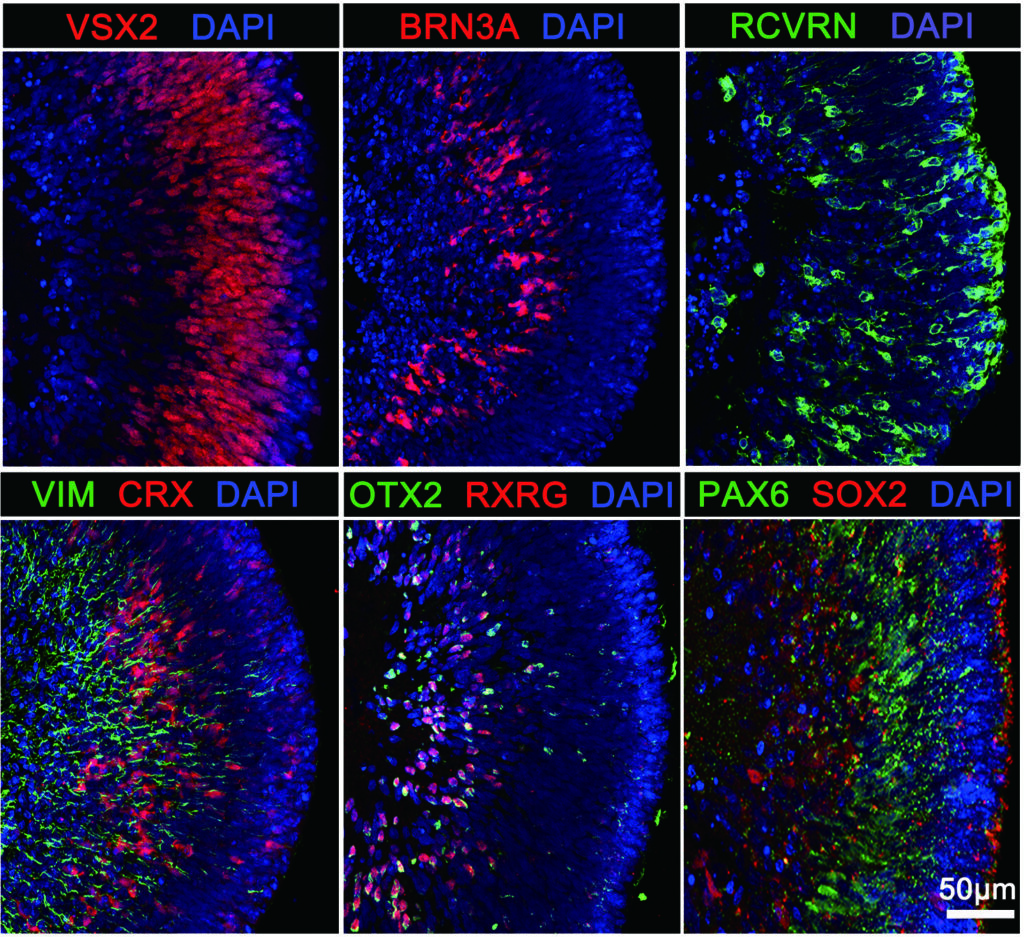
In the study, published in Science Translational Medicine, researchers employed advanced single-cell and spatial transcriptomic techniques to identify and characterize these stem-like cells in human fetal retinal tissue. They examined samples from four donors at 21 weeks of gestation, using sequencing and gene expression analysis to pinpoint the location and molecular properties of potential stem cells.
The research focused on the peripheral retina, specifically a region known as the ciliary marginal zone (CMZ). This area has been a topic of interest due to its similarities to stem cell niches found in regenerating species. By analyzing additional fetal tissue samples from donors between 16 and 22 weeks of gestation, the scientists confirmed the presence of a distinct population of neural retinal stem-like cells in this zone. These cells exhibited gene expression patterns consistent with self-renewal and the ability to differentiate into various retinal cell types.
Regeneration in Retinal Organoids and Animal Models
To further investigate the regenerative potential of these stem-like cells, researchers turned to retinal organoids—lab-grown models that mimic human retinal development. Remarkably, the same population of cells was found in the peripheral regions of these organoids, displaying overlapping genetic characteristics with those identified in human fetal tissue.
When the organoids were subjected to injury, the stem-like cells responded by migrating into the damaged area and generating new retinal cells. The gene activity observed during this repair process closely mirrored the natural development of the retina in the fetal stage. This finding demonstrated that these cells could actively participate in retinal regeneration under the right conditions.
Taking the research a step further, the scientists transplanted the human retinal stem-like cells into a mouse model of inherited retinal degeneration. Over a 24-week period, the transplanted cells integrated into the host retina, matured into functional retinal cell types, and established synaptic connections with neighboring neurons. Mice that received the transplant exhibited stronger visual responses and improved retinal structure compared to untreated controls, providing the first direct evidence of functional restoration.
Implications for Future Therapies
One of the most promising aspects of this discovery is the potential for these human retinal stem-like cells to serve as a basis for future regenerative therapies. Unlike previously studied retinal progenitor cells, this newly identified population demonstrated broader differentiation capabilities and longer-term viability. Notably, the transplanted cells did not form tumors or cause adverse effects, a crucial factor for the safety of future clinical applications.
The findings also suggest that retinal organoids could be used as a sustainable source of stem-like cells for research and therapeutic development. By refining methods for cell isolation, expansion, and transplantation, scientists may one day harness these cells to develop treatments for retinal diseases that currently have no cure.
Challenges and the Road Ahead
While this study marks a major advancement, several challenges remain before these stem-like cells can be used in human therapies. Future research will need to address key issues such as immune compatibility, the long-term stability of transplanted cells, and their effectiveness in models that more closely resemble human retinal diseases. Clinical trials will ultimately be required to determine whether these cells can provide lasting visual restoration in patients.
Despite these challenges, the identification of human neural retinal stem-like cells represents a transformative step in vision science. By unlocking the regenerative potential of the human retina, this discovery brings new hope to millions affected by vision loss and opens exciting possibilities for the future of ophthalmic medicine.
Reference: Hui Liu et al, Identification and characterization of human retinal stem cells capable of retinal regeneration, Science Translational Medicine (2025). DOI: 10.1126/scitranslmed.adp6864