For decades, patients with drug-resistant epilepsy have faced a harrowing uncertainty. When medications fail, and seizures persist, the only known cure is brain surgery—an intricate operation that depends entirely on one thing: knowing exactly where in the brain the seizures are starting. Now, thanks to groundbreaking work at Addenbrooke’s Hospital in Cambridge, a revolutionary new MRI technique is giving doctors an unprecedented view inside the brain, revealing hidden abnormalities and offering renewed hope to patients whose conditions were previously untreatable.
The 7 Tesla MRI: A Giant Leap in Brain Imaging
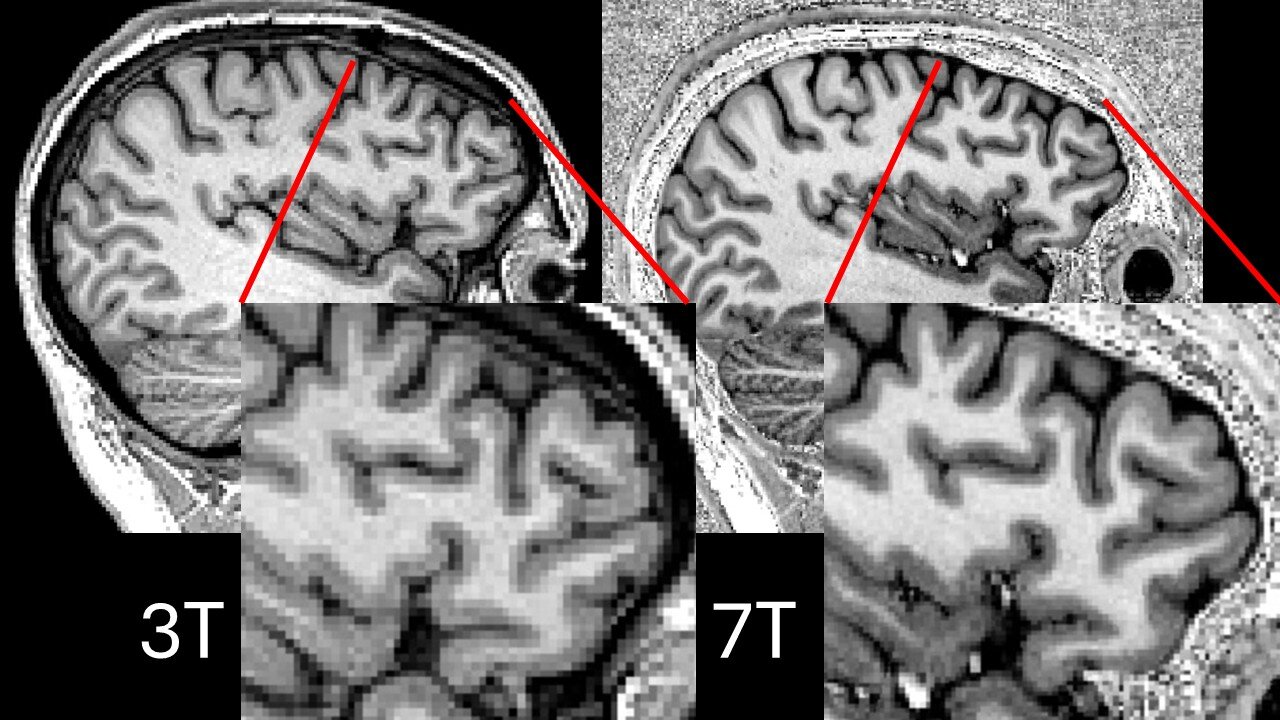
At the heart of this medical revolution is the ultra-powerful 7 Tesla (7T) MRI scanner. To put that in perspective, the standard MRI scanners found in most NHS hospitals operate at 1.5 Tesla. Some of the best machines, reserved for more complex cases, manage 3 Tesla. But the 7T scanner is more than twice as powerful—offering an unparalleled level of detail, akin to switching from an old tube TV to an ultra-high-definition display.
This technology allows neurologists to scrutinize the brain with microscopic precision, picking up subtle structural abnormalities—tiny lesions or areas of diseased tissue—that are the root cause of epilepsy in many patients. These lesions are often elusive on standard scans, hiding in plain sight, and their discovery can make the difference between an ongoing struggle with epilepsy and a life free from seizures.
The Problem with Power: Signal Dropouts in Critical Brain Regions
Despite their promise, early 7T MRI scanners came with a frustrating flaw. The increased magnetic field strength, while offering superior detail, often produced signal dropouts—blackspots where the image would fade or disappear entirely. Tragically, these dropouts often occurred in the temporal lobes, which are precisely where most focal epilepsies originate.
Imagine trying to fix faulty wiring in a house while peering through a keyhole, only to have large areas suddenly shrouded in darkness. That’s the challenge neurologists faced, even with their most powerful tools. Without a clear image, they couldn’t confidently pinpoint the epileptic lesion responsible for a patient’s seizures, leaving many patients without the option of life-changing surgery.
Parallel Transmit: A Game-Changer in MRI Imaging
Enter parallel transmit technology, an ingenious solution that has unlocked the full potential of the 7T scanner. Researchers at Cambridge’s Wolfson Brain Imaging Centre, collaborating with the Université Paris-Saclay, have successfully adapted this technique for epilepsy patients in clinical practice.
Traditional MRI scanners rely on a single radiofrequency transmitter—think of it like a lone Wi-Fi router in a large house. Just as there are areas in your home where your Wi-Fi signal weakens, single transmit MRI scanners leave parts of the brain with poor imaging quality. Parallel transmit technology replaces that single transmitter with eight, strategically positioned around the patient’s head. It’s like setting up a Wi-Fi mesh system, ensuring full coverage and eliminating those frustrating dark zones.
As Professor Chris Rodgers, Professor of Biomedical Imaging at the University of Cambridge, explains:
“Now, by using multiple radio transmitters positioned around the patients’ heads—like having a Wi-Fi mesh around your home—we can get much clearer images with fewer blackspots. This is important for the epilepsy scans because we need to see very precisely which part of the brain is misbehaving.”
Even better, the French team’s “plug-and-play” scanning sequences mean there’s no need for lengthy recalibration between patients, making the technology practical for everyday clinical use, not just high-level research.
The First Study: Real Patients, Real Results
In the first study of its kind, 31 patients with treatment-resistant focal epilepsy were scanned at Addenbrooke’s Hospital using the new parallel transmit 7T MRI. Each had been living with the relentless uncertainty of seizures that refused to be controlled by medication. For them, surgery was a tantalizing but elusive option—one that could only be offered if doctors could identify the source of their seizures.
The results were nothing short of remarkable:
- In nine patients, the 7T scans revealed previously undetectable lesions, opening the door to curative surgery.
- In four patients, the 7T images confirmed suspected lesions first spotted on 3T scans, giving surgeons added confidence.
- In another four patients, the scans debunked false positives seen on earlier MRIs, sparing them unnecessary and potentially risky surgeries.
In total, over half of the patients (18 out of 31) had their epilepsy management plans changed as a direct result of the enhanced imaging:
- Nine patients were offered surgery to remove the lesion.
- One patient underwent laser interstitial thermal therapy (LITT), a minimally invasive procedure that uses heat to destroy abnormal brain tissue.
- Five patients, with more complex lesion locations, were offered stereotactic electroencephalography (sEEG). This involves placing electrodes deep into the brain to pinpoint seizure activity—a costly and invasive procedure, but one now targeted to those most likely to benefit.
Sadly, for three patients, the clearer images revealed lesions too complex or widespread for surgery. But even that knowledge spared them from risky interventions that were unlikely to succeed.
Changing Lives: From Diagnosis to Cure
For many of these patients, the impact of the new scans is life-changing. Dr. Thomas Cope, Consultant Neurologist at Cambridge University Hospitals, highlights the transformative potential:
“Having epilepsy that doesn’t respond to anti-seizure medications can have a huge impact on patients’ lives, often affecting their independence and their ability to maintain a job. We know we can cure many of these patients, but that requires us to be able to pinpoint exactly where in the brain is the root of their seizures.”
Thanks to parallel transmit 7T MRI, more patients than ever before are now eligible for surgery that offers a cure, not just symptom management.
Patient Experience: A Comfortable, Acceptable Procedure
Despite the advanced technology and the intimidating reputation of MRI scans, patients tolerated the 7T parallel transmit scans well. The most common complaints were minor dizziness when entering the scanner and a sense of claustrophobia from the head coil—a familiar experience for anyone who’s ever had an MRI. Importantly, patients overwhelmingly found the procedure acceptable, especially given the potential benefits.
What This Means for the Future of Epilepsy Treatment
This breakthrough is not just a technical achievement—it’s a pivotal moment for the field of neurology and epilepsy surgery. Until now, 7T MRI’s potential was limited by technical hurdles that made it unreliable for clinical decisions in the most critical areas of the brain. Parallel transmit technology has smashed through that barrier.
For healthcare systems like the NHS, where resources are stretched and many hospitals still rely on older 1.5T MRI machines, the adoption of 7T technology is a leap into the future. The challenge will be in scaling up this technology—ensuring that more hospitals gain access to 7T scanners equipped with parallel transmit capability, and training radiologists and neurologists in interpreting these sophisticated images.
Beyond Epilepsy: The Wider Potential of Parallel Transmit MRI
While epilepsy surgery is the immediate focus, the implications of this breakthrough extend far beyond. Parallel transmit MRI has the potential to improve imaging across a range of neurological conditions, from brain tumors to neurodegenerative diseases like Alzheimer’s. Clearer, more detailed brain images can lead to earlier diagnoses, better surgical planning, and, ultimately, improved patient outcomes.
And as MRI technology continues to evolve, we may soon see 10.5T MRI and beyond. But without the innovations that eliminate signal dropouts—like parallel transmit—higher field strengths won’t fulfill their promise. This study shows what’s possible when advanced hardware meets equally sophisticated techniques.
In Conclusion: A Clearer Brain, A Brighter Future
The human brain is a remarkable, complex organ, and understanding its mysteries has always been one of science’s greatest challenges. For patients with drug-resistant epilepsy, those mysteries often mean a life in limbo. But with parallel transmit 7T MRI, doctors can now shed light on the darkest corners of the brain, revealing what was once invisible and offering real hope for a cure.
At Addenbrooke’s Hospital, patients who once had nowhere left to turn are now being offered surgery that could change their lives forever. And with continued research, collaboration, and investment, this could be just the beginning of a new era in brain imaging and neurosurgery.
As Professor Chris Rodgers aptly puts it,
“We need to see very precisely which part of the brain is misbehaving.”
Now, they can.