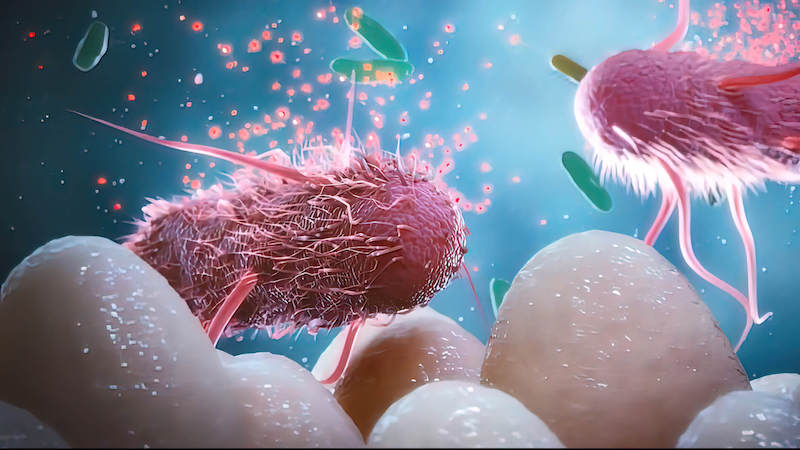
Imagine a world teeming with life, a world in which millions of organisms, too small to see with the naked eye, are constantly at work. These tiny creatures live inside of us, shape our daily lives, and influence our health in ways that were once unimaginable. This world is our gut microbiome, a vast, complex ecosystem of trillions of microorganisms—bacteria, fungi, viruses, and other microbes—that reside in our digestive system. These microbes have a profound impact on our physical, mental, and emotional well-being, acting as invisible agents of health, disease, and everything in between.
The study of the microbiome is one of the most exciting areas of modern science. It is a revolution in medicine, biology, and health that has dramatically reshaped our understanding of how the human body functions. From controlling our immune system and digesting food to influencing our mood, weight, and even our susceptibility to disease, the microbiome is emerging as one of the most powerful forces in determining our overall health.
In this article, we will explore the fascinating world of the microbiome, how gut bacteria control our health, and how modern science is beginning to understand and harness the power of these microscopic organisms.
The Gut Microbiome: What Is It?
The human microbiome refers to the trillions of microorganisms living in and on the human body. While the microbiome can be found on the skin, in the mouth, and in other parts of the body, the most densely populated area is the gut. In fact, the gut microbiome contains more than 100 trillion bacteria—many more than the number of cells in the human body. These bacteria belong to thousands of different species, and they are involved in a wide range of functions that are essential for human health.
The gut microbiome is a dynamic and complex system that interacts with the human body in numerous ways. It is not just a passive collection of microbes, but a living, breathing ecosystem that constantly communicates with the body. These microbes play an essential role in digestion, metabolism, immune function, and even brain function. They help break down food, produce essential vitamins, regulate the immune system, and protect against harmful pathogens.
While the term “microbiome” is often used to describe the collection of microbes in the gut, it also refers to the entire microbial community within the human body. This includes bacteria, viruses, fungi, and other microorganisms that live in various parts of the body. However, the gut microbiome is the most studied and perhaps the most important of these ecosystems, given its vast size and crucial role in health.
How Gut Bacteria Influence Digestion and Metabolism
One of the primary roles of the gut microbiome is in digestion. The human body cannot digest all types of food on its own, particularly complex carbohydrates like fiber. This is where the gut bacteria come in. They break down food that the human digestive system cannot process, helping to extract energy and nutrients from food.
For example, the gut bacteria play a key role in breaking down dietary fiber into short-chain fatty acids (SCFAs), which are an important energy source for the body. SCFAs, such as acetate, propionate, and butyrate, have been shown to support gut health by nourishing the cells that line the intestines, reducing inflammation, and promoting a healthy balance of gut bacteria.
The microbiome also helps the body absorb essential vitamins and minerals. Certain bacteria in the gut synthesize vitamins like vitamin K and some of the B vitamins, which are crucial for maintaining health. These microbes also help in the absorption of minerals like calcium, magnesium, and iron, ensuring that the body gets the nutrients it needs to function optimally.
In addition to digestion, the microbiome plays a crucial role in regulating metabolism. The balance of gut bacteria can influence how the body processes and stores fat, and it can even impact weight gain or loss. Emerging research suggests that an imbalance in gut bacteria—known as dysbiosis—may contribute to obesity and metabolic disorders such as type 2 diabetes. A healthy microbiome, on the other hand, is associated with a more efficient metabolism and a balanced weight.
Gut Health and the Immune System
The gut microbiome is intimately connected to the immune system. In fact, around 70-80% of the body’s immune cells are located in the gut. The gut serves as the body’s first line of defense against harmful pathogens, and the microbiome plays a central role in maintaining the integrity of this defense system.
The gut microbiome helps to train and regulate the immune system. Beneficial bacteria in the gut stimulate the production of immune cells, including T-cells and B-cells, which are responsible for identifying and attacking pathogens. These microbes also help the immune system distinguish between harmful invaders and harmless substances, preventing unnecessary immune responses that can lead to conditions like allergies or autoimmune diseases.
Furthermore, the microbiome helps maintain the gut barrier, which prevents harmful substances, such as pathogens and toxins, from entering the bloodstream. The gut lining is made up of a single layer of epithelial cells, and the microbiome helps strengthen this barrier by producing metabolites that support cell health. A healthy gut microbiome ensures that the gut lining remains intact, preventing “leaky gut” syndrome, which has been linked to a variety of health problems, including inflammatory bowel disease, food allergies, and autoimmune conditions.
Interestingly, the gut microbiome also plays a role in the development of chronic diseases, such as cardiovascular disease and cancer. Studies have shown that an imbalance in gut bacteria can contribute to inflammation, which is a key driver of many chronic diseases. By modulating the immune system and controlling inflammation, the microbiome can either protect against or contribute to the development of these conditions.
The Gut-Brain Axis: How Gut Bacteria Affect Mental Health
Perhaps one of the most intriguing discoveries in microbiome research is the connection between gut health and mental health. The gut and the brain are in constant communication through what is known as the gut-brain axis, a bidirectional signaling network that links the gut microbiome to the central nervous system.
The gut microbiome has been shown to influence brain function and behavior in a variety of ways. For example, certain gut bacteria produce neurotransmitters, such as serotonin and gamma-aminobutyric acid (GABA), that play key roles in regulating mood, anxiety, and stress. In fact, it is estimated that around 90% of the body’s serotonin, a neurotransmitter that regulates mood and happiness, is produced in the gut.
Research has also shown that the microbiome can influence the brain’s stress response. Stress can alter the balance of gut bacteria, leading to dysbiosis, which in turn can exacerbate feelings of anxiety and depression. On the other hand, a healthy microbiome can help regulate the body’s stress response, promoting resilience and mental well-being.
The gut-brain axis also explains why certain gut conditions, such as irritable bowel syndrome (IBS) or inflammatory bowel disease (IBD), are often associated with mental health issues. People with IBS, for example, are more likely to experience anxiety and depression, likely due to the disruptions in the gut microbiome and the communication between the gut and the brain.
Emerging research suggests that improving gut health may be a promising strategy for addressing mental health disorders. Probiotics, prebiotics, and other interventions that promote a healthy microbiome have been shown to have positive effects on mood, anxiety, and even cognitive function.
Gut Microbiome and Chronic Disease
The role of the gut microbiome in chronic disease is a rapidly growing area of research. An imbalanced or dysfunctional microbiome has been implicated in a wide range of health conditions, from autoimmune diseases to cardiovascular disease, diabetes, and even cancer.
One of the most significant findings in microbiome research is the association between dysbiosis and obesity. Studies have shown that individuals with obesity often have a less diverse microbiome, with an overgrowth of certain types of bacteria that promote fat storage. By contrast, individuals with a more diverse microbiome tend to have a healthier weight and metabolism. This has led researchers to investigate the potential of using probiotics, prebiotics, and dietary interventions to restore a healthy microbiome and help combat obesity.
Similarly, the microbiome has been linked to autoimmune diseases, such as rheumatoid arthritis and multiple sclerosis. Dysbiosis in the gut can lead to immune system dysfunction, causing the immune system to attack healthy tissues in the body. By restoring balance to the gut microbiome, it may be possible to reduce inflammation and improve the symptoms of autoimmune diseases.
The microbiome’s role in cardiovascular health is also becoming increasingly clear. Imbalances in gut bacteria have been associated with an increased risk of atherosclerosis, high blood pressure, and other cardiovascular conditions. The microbiome may influence cardiovascular health by regulating inflammation, blood sugar levels, and fat metabolism.
Moreover, the gut microbiome may also influence cancer development. Certain types of bacteria in the gut have been shown to produce metabolites that promote inflammation and DNA damage, which can increase the risk of cancer. On the other hand, a healthy microbiome may help protect against cancer by promoting immune function and reducing inflammation.
The Microbiome and Personalized Medicine
As we learn more about the microbiome, researchers are beginning to explore how this knowledge can be used to personalize medicine. Just as each individual has a unique genetic makeup, they also have a unique microbiome. The composition of an individual’s microbiome is influenced by a variety of factors, including diet, genetics, environment, and lifestyle. Understanding the specific makeup of an individual’s microbiome can help guide personalized treatment plans for a variety of health conditions.
For example, microbiome profiling could be used to tailor dietary recommendations, probiotics, or medications to promote gut health and overall well-being. Personalized approaches to medicine could also help identify individuals at risk for chronic diseases, such as diabetes or cardiovascular disease, based on their microbiome composition.
Conclusion: Embracing the Microbiome Revolution
The microbiome revolution is transforming our understanding of human health. We are beginning to appreciate the incredible complexity and power of the gut microbiome and its profound influence on digestion, metabolism, immunity, mental health, and chronic disease. While much remains to be discovered, the microbiome offers exciting new possibilities for disease prevention, treatment, and personalized medicine.
As we continue to explore this hidden world within us, it is becoming increasingly clear that maintaining a healthy, balanced microbiome is essential for our overall well-being. Through diet, lifestyle changes, and emerging therapies, we can take control of our microbiome and harness its power to optimize health and prevent disease.
The microbiome revolution is not just about bacteria—it’s about a new way of thinking about our health, one that recognizes the intricate interplay between our body, our environment, and the microbial world that inhabits us. As we continue to unlock the secrets of this invisible world, we will gain new insights into how to live longer, healthier, and more vibrant lives.
Think this is important? Spread the knowledge! Share now.