Cancer remains one of the most formidable challenges in modern medicine, with some tumor types notorious for their ability to spread beyond their point of origin and form metastases in distant organs. This process begins when cells from the primary tumor break free and enter the bloodstream, circulating as circulating tumor cells (CTCs). In some cases, these individual cancer cells may cluster together into small groups of up to a dozen cells, which then travel to other parts of the body. Once they settle in other organs, these clusters can grow into new, often aggressive tumors known as metastases.
Metastasis is one of the primary reasons cancer remains so difficult to treat, responsible for around seven million deaths worldwide each year. For many cancers, when metastases form, the outlook for the patient worsens dramatically. Breast cancer is a leading example of how metastatic disease severely impacts survival rates. Once breast cancer cells leave their primary site and form secondary tumors, the survival chances for patients drop significantly, and tens of thousands of women worldwide lose their lives to this aggressive form of cancer.
Given the dangerous implications of metastasis, oncologists and researchers have been tirelessly working to understand and intervene in the processes that allow these CTC clusters to spread. The goal is to disrupt these clusters before they can establish new metastatic sites, ultimately reducing the risk of secondary tumors and improving the patient prognosis. Recent progress in this direction has been encouraging, thanks to a breakthrough clinical study focused on a promising, low-cost approach to interfering with the metastasis process.
A Revolutionary Approach to Stopping Metastasis: The Power of Digoxin
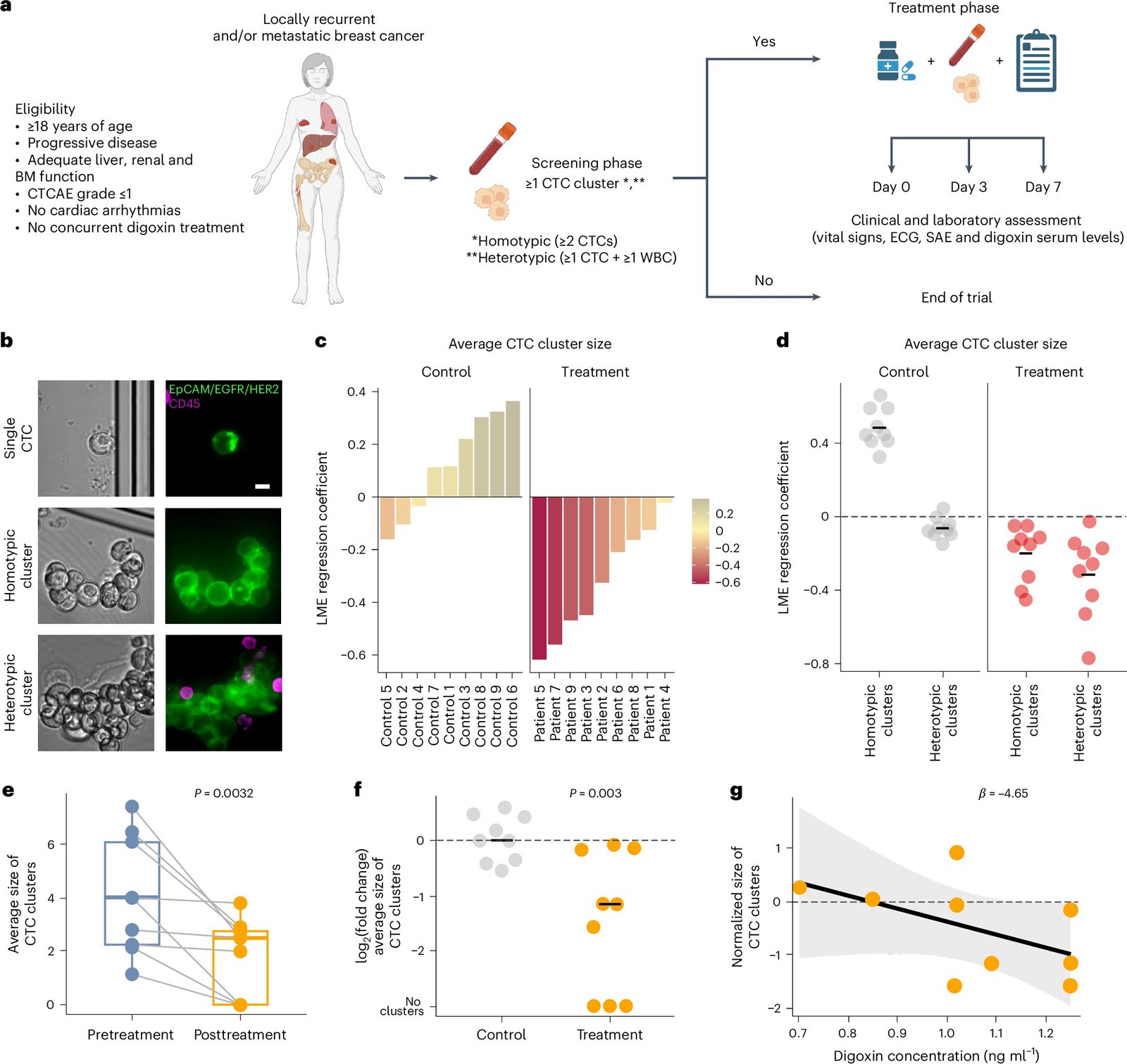
A new clinical trial published in Nature Medicine showcases the potential of a widely used cardiac drug called digoxin in limiting the spread of breast cancer. This exciting study, led by researchers from ETH Zurich, University Hospitals of Basel and Zurich, and the Basel-Land Cantonal Hospital, highlights an innovative approach to attacking the metastatic spread before it becomes too advanced.
In their research, the team administered digoxin, a drug historically used to treat conditions like heart failure, to nine patients diagnosed with metastatic breast cancer. Rather than targeting the tumor directly, the focus of the treatment was on the circulating tumor cell clusters—a critical factor in the formation of metastases.
Over the course of the study, the patients were given digoxin at a low and safe dosage for one week. The results were promising: the average size of tumor cell clusters decreased significantly, reducing by an average of 2.2 cells per cluster. While the individual size reduction might sound modest, this change has profound implications. Cancer cell clusters are typically small, often no larger than a handful of cells, and a reduction in their size directly correlates with lower metastatic potential. Smaller clusters are less able to successfully infiltrate new organs and establish secondary tumors, greatly reducing the chances of metastasis.
Why Do CTC Clusters Matter in Metastasis?
The success of metastasis is largely tied to the size and cohesiveness of these circulating tumor cell clusters. As Professor Nicola Aceto, the principal investigator of the study and Professor of Molecular Oncology at ETH Zurich, explains: “Breast cancer metastasis depends on CTC clusters. The larger they are, the more successful they are.” These clusters operate like small “pockets” of cancer that can navigate through the bloodstream, settle in distant organs, and form life-threatening tumors. By breaking up the clusters, researchers may significantly impair their ability to metastasize and start new tumors.
The molecular Achilles’ heel of these CTC clusters lies in a group of transport proteins found in the tumor cells’ membrane called sodium-potassium pumps or Na+/K+-ATPases. These pumps play an essential role in regulating the flow of ions—especially sodium and potassium—across the cell membrane, maintaining a balance of ions that is crucial for proper cell function. The pumps expel sodium from inside the cells and bring in potassium from outside.
Digoxin interferes with these pumps, blocking their function and disrupting the ion exchange. As a result, the tumor cells begin to absorb more calcium from outside their membranes. The influx of calcium weakens the connections between cancer cells in the cluster, causing them to lose their cohesion and break apart. Without the tightly formed clusters, the cancer cells struggle to spread and form metastatic tumors in distant organs.
However, digoxin doesn’t eliminate the cancer itself—it disrupts the ability of CTC clusters to form successful metastatic lesions. For this to be a truly comprehensive solution, digoxin would need to be used in combination with other therapies that target and destroy existing cancer cells.
Beyond Metastatic Breast Cancer: A Vision for Broader Cancer Applications
The implications of this study stretch far beyond just breast cancer. While breast cancer metastasis is a focus, the same basic principles apply to a range of other cancers that spread aggressively, including prostate, colorectal, pancreatic cancers, and even melanoma. In fact, Professor Nicola Aceto has already begun expanding this approach to study other cancer types. The hope is that disrupting CTC clusters might also help patients with a wide array of cancers, increasing survival chances and improving outcomes across many tumor types.
To build on these promising results, the next phase of research will be dedicated to optimizing the use of digoxin. Since the drug is already established as a treatment for heart conditions, its safety profile is well known. The next step is to further refine and enhance its ability to break down CTC clusters. Researchers are already working on the development of new molecules based on digoxin, which would perform even more effectively at reducing metastasis.
One exciting avenue for advancing the research is a spin-off company from ETH Zurich called Page Therapeutics, which is focused on further developing digoxin-based solutions. The company aims to create next-generation drugs that can more effectively dissolve these circulating tumor cell clusters, thus presenting more potent preventive treatments for metastatic cancers.
Collaboration Between Academia and Hospitals: A Model for Success
This study stands as a remarkable example of the productive collaboration between academic research institutions and medical hospitals. The team of researchers at ETH Zurich partnered closely with University Hospitals of Basel and Zurich as well as the Basel-Land Cantonal Hospital. The hospital partners were not just involved in providing the necessary clinical trial data but also played a crucial role in recruiting patients and carrying out the real-world clinical studies. Such collaboration is essential for turning promising laboratory research into effective treatments for cancer patients around the world.
The potential of digoxin in targeting circulating tumor cells is just the beginning. As the medical field continues to innovate, combining targeted therapies like this one with advanced cancer treatments may drastically change the prognosis for cancer patients, especially those with metastatic disease.
Conclusion: A New Hope for Cancer Patients
The promising results of this clinical trial offer a glimpse into a future where metastatic cancer may no longer be as dire a diagnosis as it has historically been. By targeting the early steps in metastasis—preventing cancer cells from forming effective clusters in the bloodstream—researchers have taken a critical step toward curbing the spread of some of the most aggressive and deadly cancers.
While this treatment alone does not eliminate existing tumors, it offers a path forward in reducing metastatic risk and improving patient outcomes, especially when combined with other therapies that target tumor cells directly. The ongoing work to optimize the effectiveness of digoxin and other agents will play a crucial role in creating more comprehensive and impactful treatments in the years to come.
This research underscores the importance of collaborative, cross-disciplinary efforts in making strides against cancer, especially as the scientific community shifts its focus toward better understanding, preventing, and managing metastatic disease. With further research and innovation, we may be on the cusp of a new era of cancer treatment—one where patients are better equipped to fight back against metastasis and achieve longer, healthier lives.
Reference: Christian Kurzeder et al, Digoxin for reduction of circulating tumor cell cluster size in metastatic breast cancer: a proof-of-concept trial, Nature Medicine (2025). DOI: 10.1038/s41591-024-03486-6. www.nature.com/articles/s41591-024-03486-6