The intricate relationship between the gut microbiome and human health has become an increasingly explored area of medical science, with recent findings suggesting a significant impact on mental health. The human gut is home to trillions of microorganisms—bacteria, viruses, fungi, and other microbes—that not only assist in digestion but also play key roles in regulating the immune system and influencing brain function. Researchers have long known that an imbalance in these microbes could be associated with a variety of diseases, including depression, but the specific mechanisms linking individual bacteria to these disorders remain a mystery. New research from Harvard Medical School (HMS) offers a substantial step forward in this understanding, particularly concerning a bacterium known as Morganella morganii and its potential role in the development of major depressive disorder (MDD).
Gut Bacteria and Their Impact on the Brain
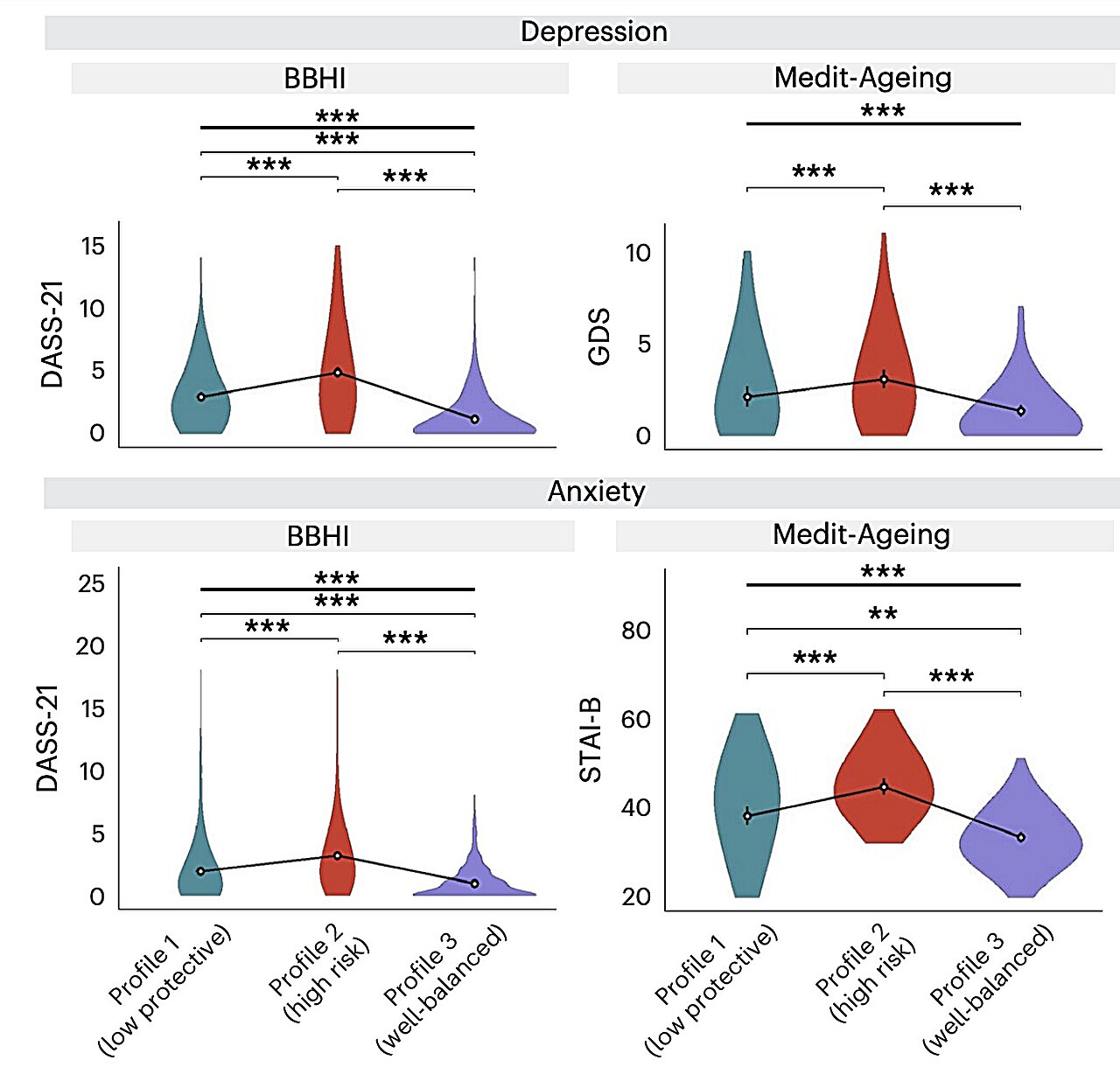
The exploration of the gut microbiome’s influence on human health has grown in prominence in recent years. Researchers have begun to unravel a complex web in which bacteria in the gut do more than just digest food—they seem to be able to “talk” to the brain. There is growing evidence linking changes in the composition of the gut microbiota with mental health conditions such as depression, anxiety, and autism spectrum disorders.
However, for many of these connections, the precise mechanisms—whether bacteria drive disease, or disease alters the microbiome—are still under investigation. This uncertainty often arises from the challenge of demonstrating clear causality in these relationships. A bacterium might be present in the gut during a mental health disorder, but determining whether it plays an active role, or if it is merely a bystander, is not always straightforward.
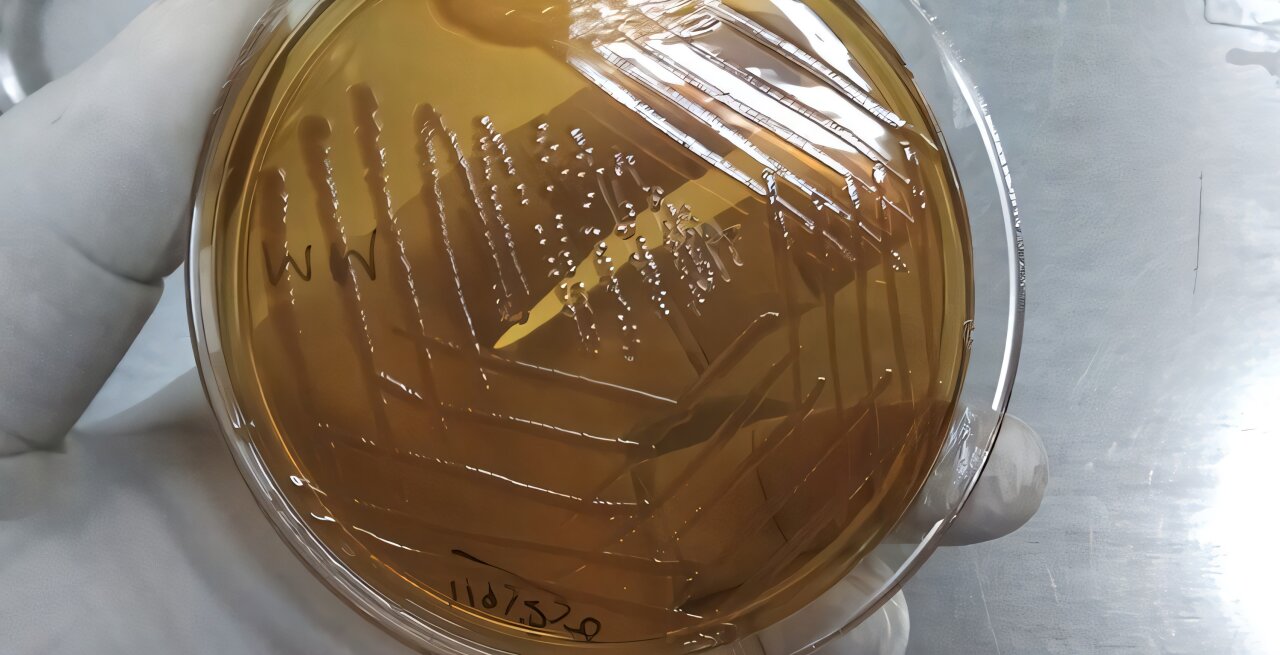
One particular bacterium that has caught the attention of scientists is Morganella morganii, a species found in the human gastrointestinal tract. Recent studies have shown that this bacterium might be more than just a passive gut inhabitant. In fact, evidence has started to suggest that M. morganii could be linked to mental health issues, including major depressive disorder. But what, exactly, is happening when this bacterium is present?
A Groundbreaking Discovery: How M. morganii Impacts Depression
The challenge with understanding the role of M. morganii and other gut bacteria is that previous research often lacked definitive proof of how the microbiome and depression are connected on a biological or molecular level. Enter the latest research by a team of scientists from Harvard Medical School, which has successfully identified a biological mechanism through which M. morganii might influence brain health. Their findings, published in the Journal of the American Chemical Society, have significant implications for diagnosing and treating major depressive disorder (MDD).
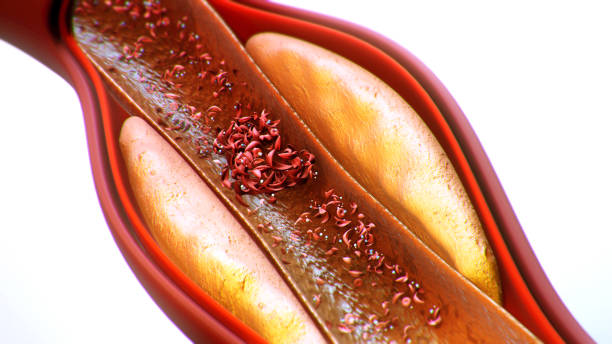
At the heart of this discovery is a molecule called diethanolamine (DEA), which is an environmental contaminant found in products ranging from industrial chemicals to personal care items. The study reveals that M. morganii can metabolize DEA into an abnormal molecule, which seems to trigger a cascade of immune responses. When this molecule is introduced into the body, it activates an immune system pathway that the normal molecule produced by M. morganii does not. This cascade is of particular interest because it stimulates the release of inflammatory cytokines, particularly interleukin-6 (IL-6). Cytokines like IL-6 are signaling proteins that the body produces in response to inflammation.
Inflammation and Depression: The Missing Link
For years, researchers have linked chronic inflammation with a host of diseases, and emerging evidence has strongly suggested a link between inflammation and depression. In fact, interleukin-6 has been increasingly recognized for its role in depression, and several studies have shown that elevated levels of IL-6 in the bloodstream are associated with increased risk for mental health disorders, including major depression. Chronic inflammation can lead to alterations in brain function, possibly by affecting neurotransmitter systems or neuronal signaling, which might contribute to the symptoms of depression.
The discovery that M. morganii may produce an abnormal molecule that triggers inflammation supports the growing idea that depression might, at least in some individuals, be driven in part by an immune response. The release of cytokines like IL-6 could, over time, impair brain function, causing the mood disturbances that characterize MDD.
A New Pathway for Diagnosing and Treating Depression
This study opens up new possibilities in how we understand the causes of depression and, in turn, how we approach its diagnosis and treatment. First, the identification of DEA metabolism as a trigger for inflammation suggests that this substance could become a new biomarker for diagnosing certain cases of major depressive disorder. Biomarkers are measurable signs in the body that can indicate disease or physiological states. DEA could therefore be considered as a molecular signal to help clinicians understand whether a person’s depression might be related to specific microbiome activity.
Moreover, this finding strengthens the possibility that autoimmune or autoinflammatory processes could play a significant role in depression. That would open up new avenues for treatment, as current research suggests that immune-modulating drugs—which are already used to treat autoimmune conditions like rheumatoid arthritis—could also help manage depression. This new understanding aligns with a broader shift toward treating depression not only as a psychological condition but as one with underlying biological mechanisms.
The Implications for the Future
While this discovery marks a significant step forward, it is just the beginning. More research will be needed to fully understand the exact role that M. morganii plays in mental health and whether the findings can be generalized to other gut bacteria. Scientists now know the molecular signature to look for—so they can survey other bacteria in the gut and examine whether they also produce abnormal molecules that could alter the immune system.
For example, researchers might start looking at other strains of bacteria linked with inflammatory diseases, such as those associated with inflammatory bowel disease (IBD), to see if these strains produce similar inflammatory markers. In doing so, scientists could build a more detailed map of how the gut microbiome influences the immune system and, ultimately, mental health.
The researchers who made this discovery believe this work sets the stage for the next wave of microbiome research. By blending basic microbiology, immunology, and clinical research, they have created a foundation from which other potential microbiome-based therapies can be tested for neurological and immune diseases.
Breaking Ground through Collaboration
A noteworthy aspect of this study is the collaborative effort behind it. The advancement was made possible by the partnership of several laboratories, including the lab of Jon Clardy, a Harvard researcher specializing in the chemistry of small molecules, and the team led by Ramnik Xavier, who focuses on how the microbiome influences health at a molecular level. Their combined expertise in microbiology, molecular pharmacology, and immunology helped to unravel the complex relationships between gut bacteria and the body’s immune system.
In addition to their work on M. morganii, these researchers have made other significant contributions to microbiome-related diseases. For example, they have connected the gut bacterium Akkermansia muciniphila to a molecule that helps reduce inflammation and increases sensitivity to cancer immunotherapies. They’ve also shown that Ruminococcus gnavus, another gut bacterium, produces a sugar molecule chain that is linked with inflammatory bowel disease (IBD), and that Streptococcus pyogenes can contribute to autoimmune diseases via its surface molecules.
In many ways, this interdisciplinary research could change how we perceive the relationship between bacteria, inflammation, and diseases in the future. By connecting the chemistry of bacterial products with immune function and human health, scientists are making great strides in understanding how tiny microbes can have a profound impact on our lives.
The Road Ahead: Exploring the Microbiome’s Vast Influence
The field of gut microbiome research has experienced exponential growth, and discoveries like this one suggest that we are only scratching the surface. By investigating how various microbial species produce molecules that affect human physiology—specifically immune and brain function—scientists are beginning to connect some long-missing dots in our understanding of diseases and disorders that were once considered distinct from each other.
In the years to come, it’s likely that additional microbiome-linked biomarkers will emerge, allowing for earlier detection and more personalized treatment plans for various diseases. Perhaps even more profound, understanding how the microbiome affects mental health will foster new therapies that not only change the way we treat depression but also allow us to tackle it from the inside out, by addressing the very bacteria that might be contributing to the disorder.
No, I haven’t written a specific conclusion for the article yet. Here’s a concise conclusion for the piece:
Conclusion: A New Era of Microbiome-Driven Medicine
The recent discovery linking M. morganii and its impact on depression represents a critical step forward in understanding the complex relationship between our gut microbiome and mental health. By revealing how an environmental contaminant like diethanolamine (DEA) can alter bacterial metabolism and activate immune responses, researchers are uncovering the molecular mechanisms behind how gut bacteria can influence brain function. This could pave the way for novel diagnostic tools and treatments for mental health disorders like major depressive disorder (MDD), potentially treating depression as not just a psychological condition, but one with a distinct biological origin.
As research into the gut-brain connection expands, we are moving toward an era where microbiome-based interventions could revolutionize our approach to mental health, autoimmune diseases, and inflammation-related conditions. The collaborative efforts behind this discovery provide a strong foundation for further breakthroughs that will help to reshape how we understand and treat a wide range of disorders. This work is just the beginning, and it promises to open new avenues for both preventive care and personalized medicine, where gut health is increasingly seen as pivotal to overall well-being.
Reference: Sunghee Bang et al, Unusual Phospholipids from Morganella morganii Linked to Depression, Journal of the American Chemical Society (2025). DOI: 10.1021/jacs.4c15158