Researchers at the University of Pittsburgh have made significant strides in asthma research by developing a nasal swab test that can identify specific subtypes, or endotypes, of asthma in children. This innovative, non-invasive diagnostic tool has the potential to transform how clinicians treat asthma by enabling more targeted medication prescriptions. It also sets the stage for better treatment development, particularly for lesser-studied asthma types that have historically been challenging to diagnose accurately.
The study, published in the prestigious medical journal JAMA, builds on data from three U.S.-based studies. These studies primarily focused on Puerto Rican and African American youths, groups that bear a disproportionately high burden of asthma and experience higher mortality rates from the disease than their non-Hispanic white counterparts.
Asthma is the most common chronic childhood disease and poses significant healthcare challenges due to its variability in severity and response to treatment. According to Dr. Juan Celedón, senior author of the study and a professor of pediatrics at the University of Pittsburgh, this variability necessitates precise diagnosis and tailored treatments. Celedón emphasizes the importance of understanding asthma endotypes—subcategories of the disease driven by distinct immune responses. This differentiation is crucial because different endotypes respond differently to treatments, and conventional approaches have often failed to address the nuances of these variations effectively.
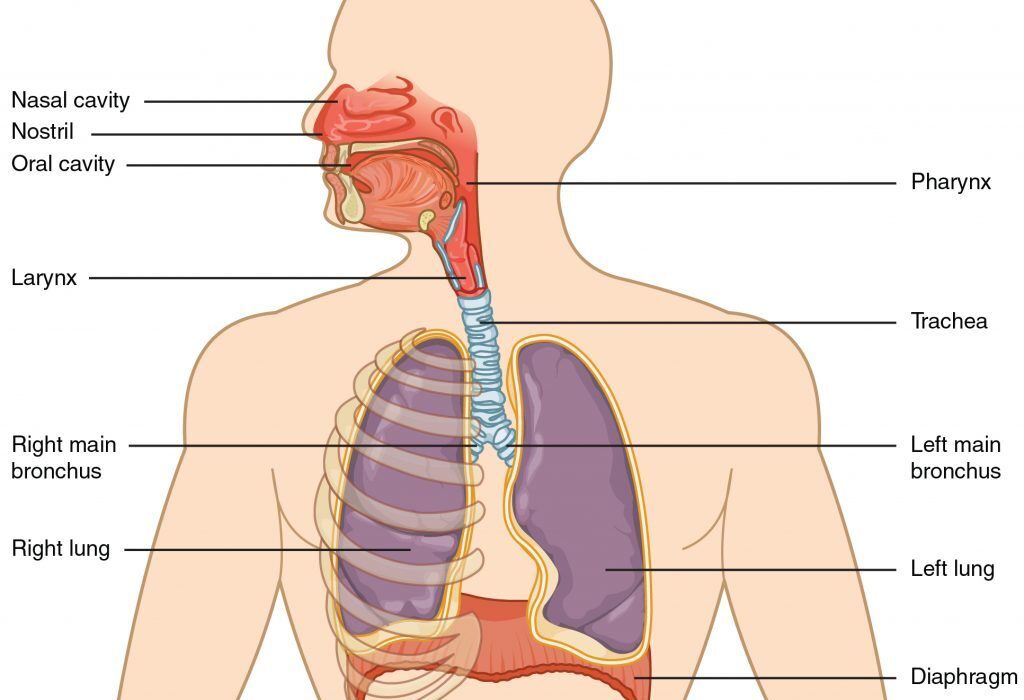
Asthma has traditionally been categorized into T2-high or T2-low endotypes based on T helper 2 (Th2) inflammation levels. However, T2-low has recently been further divided into two subtypes: T17-high, characterized by Th17 inflammation, and low-low, with minimal inflammation of both types. The current gold standard for determining endotype involves genetic analysis of lung tissue samples obtained through bronchoscopy under general anesthesia. While effective, this invasive procedure is neither feasible nor ethical for use in children, especially those with milder asthma. Consequently, clinicians have relied on less precise diagnostic tools, such as blood markers, lung function tests, and allergy assessments, which fail to offer a complete picture and cannot differentiate between T17-high and low-low endotypes.
The Pittsburgh research team, motivated by the limitations of existing methods, sought to develop a more accurate and child-friendly diagnostic approach. Led by Celedón, the group included Pitt graduate student Molin Yue and pediatrician Kristina Gaietto. The researchers analyzed nasal swab samples from 459 children across three independent studies. By studying the expression of eight signature genes linked to T2 and T17 inflammation, they successfully identified patients’ specific asthma endotypes. Remarkably, the nasal swab test identified T2-high, T17-high, and low-low endotypes with consistency across studies, with respective distributions of 23–29%, 35–47%, and 30–38%.
This advancement holds immense promise for clinical practice. For T2-high asthma, biologic treatments targeting specific immune cells driving inflammation already exist. These drugs have revolutionized care for severe cases of this subtype. In contrast, no targeted biologics currently exist for T17-high or low-low asthma, largely due to the lack of diagnostic tools capable of accurately identifying these endotypes. Celedón believes the new nasal swab test could spark a wave of research and innovation, ultimately leading to the development of biologics tailored to these understudied forms of asthma.
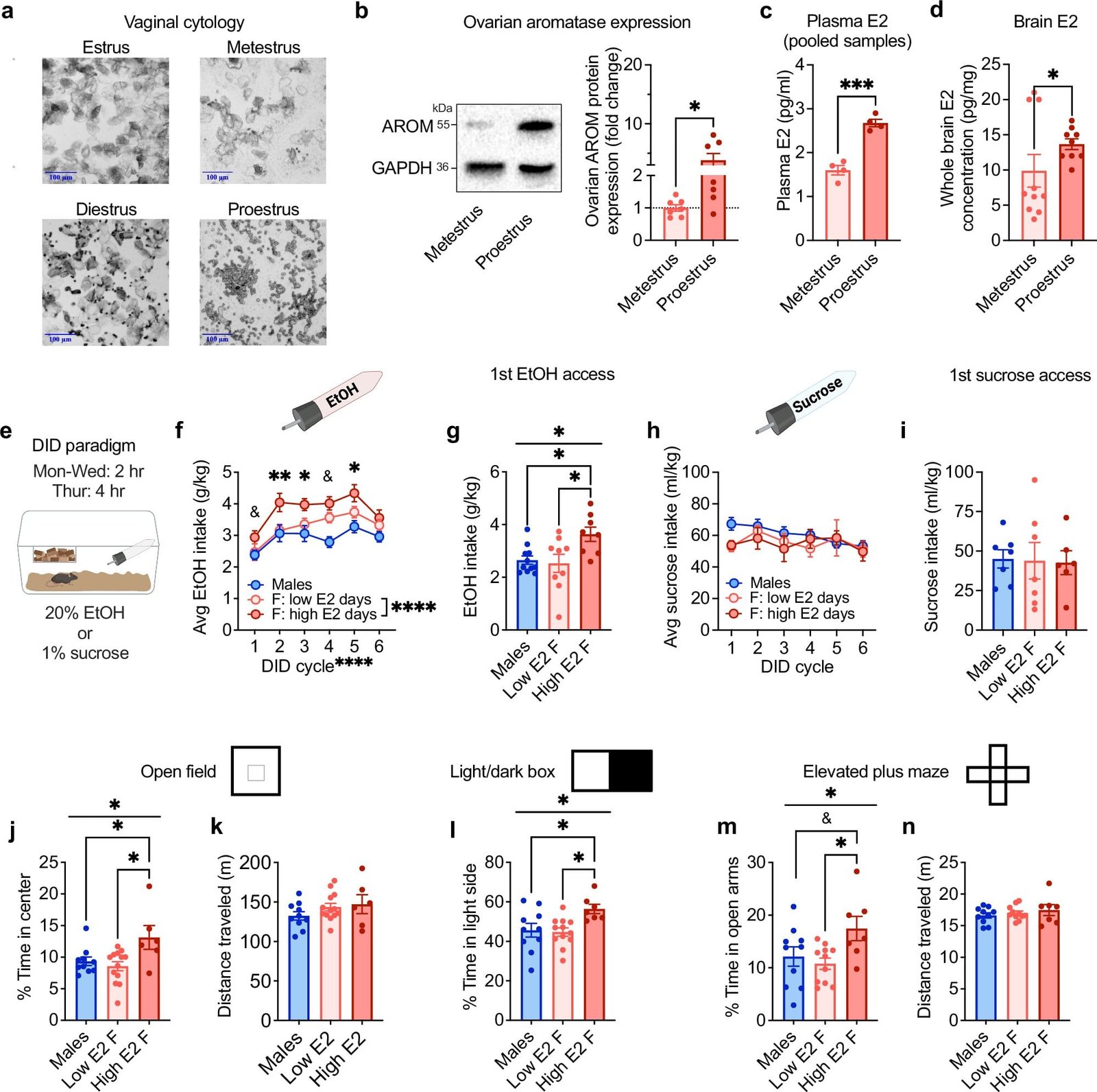
Beyond improving treatment precision, this test offers researchers a valuable tool for investigating broader questions in asthma biology. One significant area of interest is how asthma changes during puberty. Asthma incidence differs between sexes across the lifespan: boys are more frequently affected in childhood, but asthma rates rise among females in adulthood. Scientists have long speculated about the role of endotypes in these trends, but the lack of accessible diagnostic methods has stymied progress. Celedón suggests that with the availability of a reliable nasal swab test, researchers can begin exploring whether endotypes evolve over time or in response to treatment, shedding light on puberty-related shifts in asthma prevalence and severity.
The implications of this research extend beyond individual patient care. Asthma disproportionately affects minority populations, with Black and Puerto Rican children facing greater challenges and poorer outcomes. By offering a simple and effective diagnostic tool, the nasal swab test has the potential to narrow health disparities and bring personalized asthma care to underserved communities. Gustavo Matute-Bello, acting director of the Division of Lung Diseases at the National Heart, Lung, and Blood Institute, underscored the significance of this development, emphasizing its potential to improve asthma outcomes in children who experience a disproportionate disease burden. He called for further studies to capitalize on the test’s promise and drive progress toward personalized asthma care.
The study’s success is attributable to the collaborative efforts of a multidisciplinary team. Alongside Celedón, Yue, and Gaietto, the research involved contributions from Yueh Ying Han, Franziska J. Rosser, Zhongli Xu, Christopher Qoyawayma, Erick Forno, and Wei Chen, all affiliated with Pitt and UPMC. Additional co-authors included Edna Acosta-Perez and Glorisa Canino from the University of Puerto Rico, highlighting the study’s commitment to addressing the unique challenges faced by Puerto Rican children.
Asthma, as a multifaceted disease, demands innovative approaches to diagnosis and treatment. By enabling accurate identification of asthma endotypes through a non-invasive and widely accessible test, this research paves the way for significant advancements in personalized medicine. It not only holds the potential to improve outcomes for children currently struggling with asthma but also opens new avenues for understanding the disease’s underlying biology and evolution. As researchers continue to refine and expand upon these findings, the future of asthma care appears brighter and more inclusive.
Reference: Molin Yue et al. Transcriptomic profiles in nasal epithelium and asthma endotypes in youth, JAMA (2025). DOI: 10.1001/jama.2024.22684