Psychiatric disorders often show significant overlap, making their diagnosis and treatment particularly complex. Conditions like depression and anxiety often co-occur and share symptoms, while others, such as schizophrenia and anorexia nervosa, can overlap in unexpected ways. Similarly, autism spectrum disorder (ASD) and attention deficit/hyperactivity disorder (ADHD) exhibit a degree of symptomatology that can be confused with one another. The question arises: Why do these psychiatric disorders overlap so frequently?
There are several contributing factors to this phenomenon, and one of the most important is the shared genetic underpinnings that span these conditions. Genetic variations that influence psychiatric health could be acting across multiple disorders, providing common threads that link them. Although environmental and experiential factors such as trauma and stress are central to understanding psychiatric conditions, a growing body of research indicates that much of this overlap might be genetically driven. Over the past few years, a number of breakthrough studies have uncovered that there are specific genetic hotspots associated with multiple psychiatric disorders, providing insight into why certain conditions often occur together.
The Genetic Basis of Psychiatric Co-occurrence
In 2019, a collaborative study conducted by researchers from the Psychiatric Genomics Consortium (PGC), Harvard University, and the UNC School of Medicine identified 136 specific locations within the human genome—often referred to as “hotspots“—that are associated with eight major psychiatric disorders. These included autism spectrum disorder (ASD), attention deficit/hyperactivity disorder (ADHD), schizophrenia, bipolar disorder, major depressive disorder, Tourette syndrome, obsessive-compulsive disorder (OCD), and anorexia nervosa. Interestingly, 109 of these hotspots were found to be shared across several of these disorders, an observation that pointed to genetic overlap between different conditions—a concept known as pleiotropy.
While these findings were groundbreaking, there were still unanswered questions. Notably, it was unclear exactly how these shared genetic factors contributed to the specific symptoms and traits of each disorder. Researchers struggled to differentiate between those variants that were only related to one disorder and those that influenced multiple conditions. Recent advancements, however, have provided new clarity, thanks to more sophisticated methods for studying genetic interactions in living systems.
Examining Genetic Variants with a New Approach
A new study led by Hyejung Won, Ph.D., and Patrick Sullivan, M.D., from the UNC School of Medicine and the UNC Neuroscience Center has brought us closer to understanding the genetic variants that contribute to both individual and overlapping psychiatric disorders. Published in Cell, this research provides key insights into the functional role of genetic variants shared between multiple disorders.
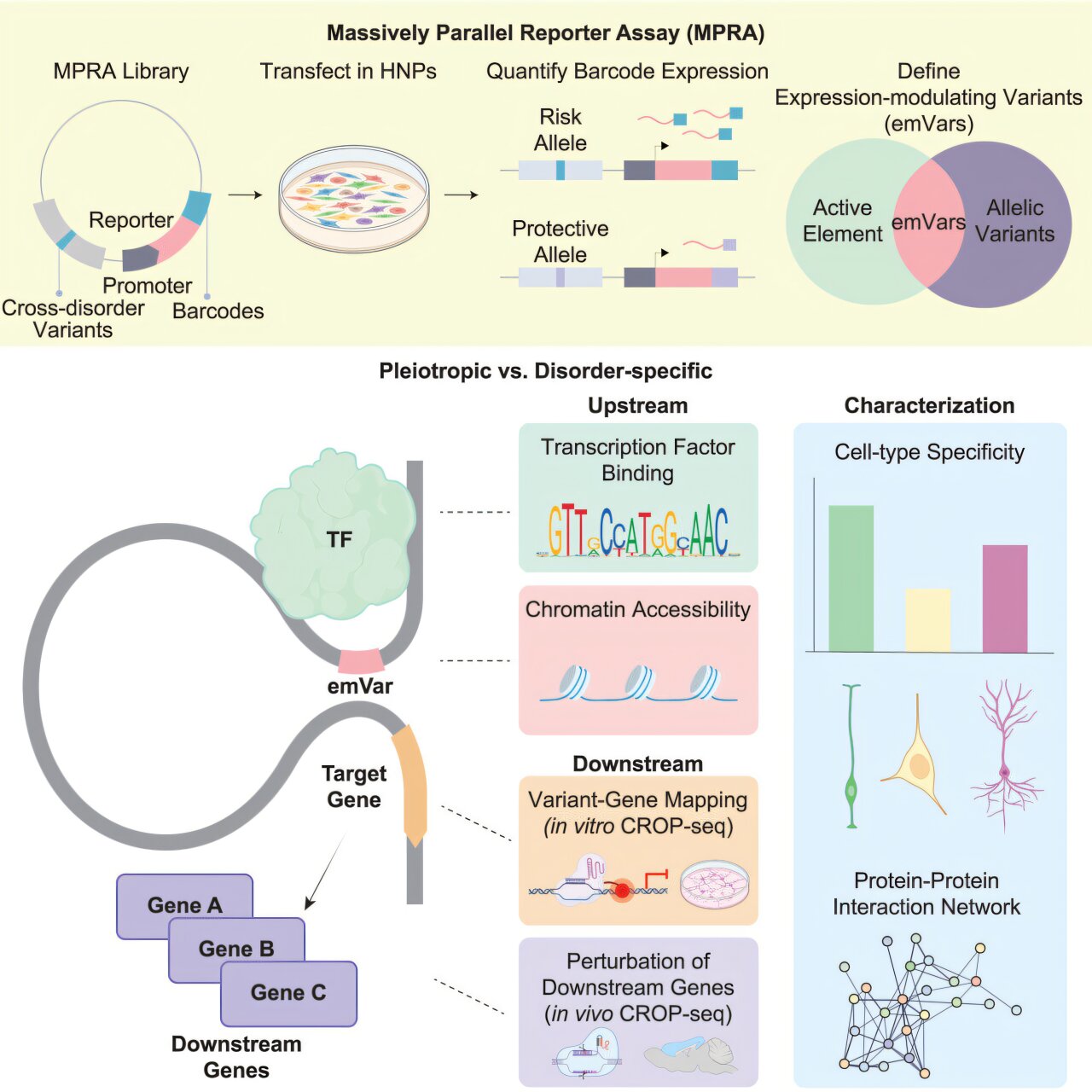
Unlike earlier studies, which focused on finding genetic variants linked to diseases in a static manner, the new study utilized advanced techniques, such as the massively parallel reporter assay (MPRA), which tracks how genetic variants behave in living human cells. This allowed the researchers to test 17,841 genetic variants from the 136 hotspots identified in the earlier research. What they found was remarkable: 683 of these variants had a measurable effect on gene regulation. Gene regulation, which controls how and when genes are turned on or off to produce proteins, is essential to proper biological functioning—alterations in this process can lead to major disruptions in mental and physical health.
The critical step of this study involved categorizing the variants based on whether they were pleiotropic (shared across multiple disorders) or disorder-specific (unique to a single disorder). Researchers then compared the two groups to gain a better understanding of their respective roles in psychiatric conditions.
Pleiotropy: A Key Target for Treatment
What the researchers uncovered was particularly valuable for advancing treatment strategies. The variants that were shared across multiple disorders—known as pleiotropic variants—were found to be not only more active, but also more sensitive to changes. These pleiotropic variants were associated with genes that were highly influential in multiple stages of neurodevelopment, affecting both the development of the brain as well as ongoing brain function.
This heightened activity suggests that pleiotropic variants could contribute to a variety of psychiatric conditions. Furthermore, these variants were active for longer periods during brain development than variants specific to a single disorder, implying that they might influence multiple traits across different psychiatric conditions. These variants seem to have a more profound impact on the development of the central nervous system (CNS) and the nervous system’s complex mechanisms—such as synapse formation and protein production—which are critical processes involved in psychiatric disorders.
Moreover, the pleiotropic genes were discovered to be intricately connected to other genes, meaning that disturbances in these genes have the potential to cause cascading effects throughout the brain. This discovery opened up exciting prospects for treating psychiatric disorders by targeting not only individual diseases, but also these key shared genes that overlap across conditions.
“The proteins produced by these pleiotropic genes are highly connected,” says Hyejung Won. “Changes to these proteins, in particular, could ripple through the network, affecting many aspects of brain development and function, potentially leading to disorders across multiple domains.”
This finding is crucial for treatment development, as it suggests that pleiotropic variants might be ideal targets for new, targeted therapies. By understanding these common genetic mechanisms, scientists could create drugs or interventions that simultaneously address multiple disorders.
Disorder-Specific Variants: Focus for Tailored Interventions
On the other side, the disorder-specific variants that are exclusive to one condition were found to be less sensitive to change and had shorter activity windows in brain development. These variants may not play as wide-reaching a role in neurological changes as pleiotropic variants, but their specific targeting could still provide benefit in treating specific psychiatric conditions.
Treatments that focus on targeting disorder-specific variants could provide more precision in how we approach individual diseases. For example, a therapy aimed at altering gene activity tied only to schizophrenia would not have the broader implications for other psychiatric disorders but would target the disorder’s unique biological components. Such tailored interventions are more likely to achieve focused clinical benefits.
However, the significant role of pleiotropic variants means that the future of psychiatric treatment may not solely rest on single-condition, disorder-specific approaches. Researchers must balance between discovering treatments for individual disorders and developing therapies that can address the shared genetic causes of psychiatric overlap.
The Promise of Future Treatments
These findings demonstrate that psychiatric genetics holds untapped promise. Targeted therapies that address the genetic variants shared across conditions, coupled with customized treatments for specific disorders, can revolutionize psychiatric medicine. Instead of treating each disorder in isolation, personalized medicine offers an approach where genetic understanding of an individual patient’s condition could lead to better diagnostic accuracy and treatment efficacy.
The challenge, of course, is that psychiatric disorders are incredibly complex and multifactorial, influenced not only by genetics but by environmental stressors, life experiences, and other external factors. Therefore, while genetics offers invaluable insight into the nature of psychiatric co-occurrence, it will always be one aspect of a much larger picture of disease.
Nevertheless, these promising results provide optimism. By harnessing the power of genetic insights, researchers are steadily unlocking the possibility of effective, multi-target treatments that could be tailored to individuals suffering from different psychiatric conditions, which, in turn, could relieve the emotional, psychological, and social burden on those affected.
As research in psychiatric genetics continues to advance, and our understanding of the intricate relationship between genetics and disease expands, we may one day be able to look beyond conventional diagnostic categories to find ways to treat the person, rather than just the diagnosis.
Conclusion
The complexity of psychiatric disorders, their often shared symptoms, and overlapping genetic factors makes them challenging to diagnose and treat. However, breakthrough research like the recent study led by Hyejung Won and Patrick Sullivan brings us closer to understanding the shared genetic mechanisms that underlie coexisting disorders. These discoveries shed light on the powerful role of pleiotropic variants, which could hold the key to developing treatments that target multiple psychiatric disorders at once, offering hope for individuals living with mental health conditions. While there is still much work to be done, the future of psychiatric genetics offers the possibility of personalized treatments, based on a more complete understanding of the genetic factors driving psychiatric illnesses, paving the way for effective and integrated therapeutic solutions.
Reference: Sool Lee et al, Massively parallel reporter assay investigates shared genetic variants of eight psychiatric disorders, Cell (2025). DOI: 10.1016/j.cell.2024.12.022