Sepsis is a life-threatening condition responsible for an estimated 8 million deaths worldwide each year. Characterized by the body’s extreme response to infection, it can lead to widespread inflammation, organ failure, and problems with blood clotting. Despite its severity, sepsis remains difficult to treat, with limited advancements in targeted therapies over the past few decades. However, a new breakthrough from researchers at Oregon Health & Science University (OHSU) is offering hope for improved treatments, potentially changing the course of sepsis management.
The OHSU team, led by Dr. Owen McCarty, Ph.D., a professor of biomedical engineering at the OHSU School of Medicine, has made significant strides in understanding how blood clotting plays a role in sepsis. Their research focuses on how certain molecules found in bacteria trigger abnormal blood clotting in sepsis, which can lead to fatal complications. By targeting these mechanisms, the team hopes to develop new therapies to better manage the disease in critically ill patients.
The Science of Sepsis and Blood Clotting
Sepsis occurs when the body’s immune system overreacts to an infection, causing a cascade of damaging effects. In this state, the body may produce excessive blood clots, which can block blood vessels and cause damage to organs like the kidneys, heart, and liver. On the other hand, as the clotting system becomes overwhelmed, the body may also experience excessive bleeding, making it a delicate balance to manage.
The underlying cause of these disruptions is often a bacterial infection. Gram-negative bacteria, such as E. coli, are common culprits in sepsis, releasing molecules like lipopolysaccharide (LPS) when they invade the bloodstream. LPS, a component found on the surface of many bacteria, is known to be a potent activator of the immune response, triggering inflammation and blood clotting.
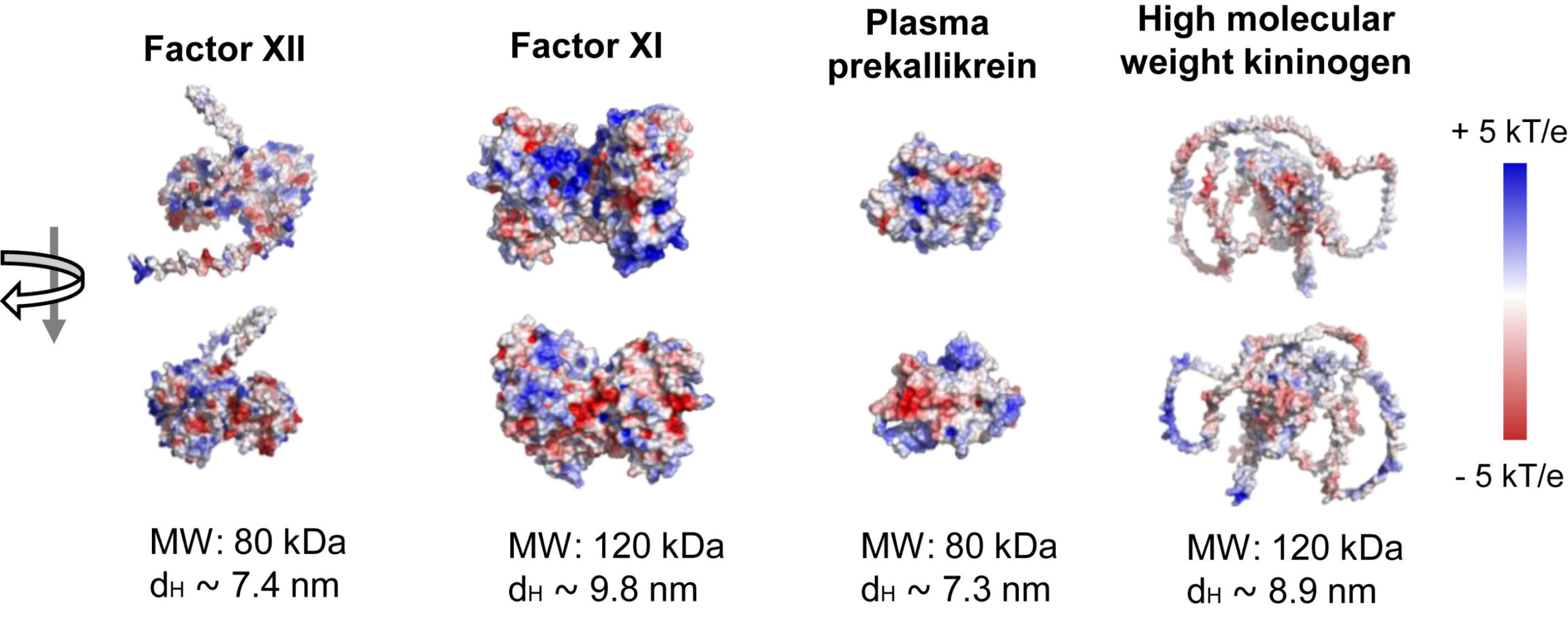
The OHSU team’s research focuses on understanding how LPS, specifically the O26:B6 strain, can directly influence blood clotting mechanisms. They discovered that LPS plays a key role in triggering the “contact pathway” of blood clotting, a process that leads to the formation of clots. In this pathway, blood proteins like factor XII work together to initiate clotting, which can be beneficial in some cases, but in the case of sepsis, it becomes dangerous and uncontrollable.
Dr. McCarty explained the basic functioning of the clotting system, saying, “Normally, the blood forms tiny clots to contain bacteria and help clear them from the bloodstream. However, when the infection overwhelms the system, it can lead to catastrophic results, with both clotting and bleeding occurring simultaneously.”
Focus on Factor XII and Potential New Treatments
One of the most significant findings of this study is the role of factor XII, a protein involved in initiating the clotting process. While most people have no issues with factor XII, those born without it do not experience abnormal bleeding or clotting issues, suggesting that targeting this protein could prevent dangerous clotting without causing harmful side effects like excessive bleeding. This presents a unique opportunity for targeted therapy.
Dr. Joseph Shatzel, M.D., a physician-scientist at OHSU who specializes in clotting and bleeding disorders, emphasized the importance of focusing on previously overlooked components of the clotting system. “Our research has concentrated on the contact activation system, which traditionally has been neglected in the development of sepsis treatments,” he said. Shatzel is particularly passionate about translating lab innovations into real-world treatments for patients, and his efforts involve direct collaboration between OHSU’s research labs and patient care facilities.
In nonhuman primates, the team demonstrated that LPS triggers the activation of factor XII, sparking a chain reaction that leads to excessive clotting. “Factor XII could be a great target for therapies to stop dangerous clotting without the risk of bleeding, as we have seen with individuals lacking this protein,” Shatzel added.
A New Approach to Sepsis Treatment
Currently, sepsis treatment largely revolves around antibiotics and supportive care to manage the infection and stabilize the patient. While this approach has helped improve survival rates, it has not fundamentally altered the high mortality rate of the condition. The OHSU team’s research is aimed at developing more effective, targeted therapies that address the clotting aspect of sepsis directly.
One of the most promising experimental treatments developed by the team involves antibodies designed to block factor XII activity. These antibodies, created at OHSU, have shown promising results in early-stage clinical trials and animal models. André L. Lira, Ph.D., a postdoctoral scholar and lead author of the study, explained, “Our research focuses on how bacterial surfaces, particularly the lipopolysaccharides found in certain bacteria, trigger clotting. By understanding these triggers, we hope to develop precision therapies tailored to specific bacterial strains.”
In addition to targeting factor XII, the team is exploring other potential clotting factors, such as factor XI, which was the subject of a separate clinical trial published in 2023. By addressing these key players in the clotting cascade, the researchers hope to mitigate the harmful clotting without impairing the body’s ability to heal.
“We are optimistic that our approach could prevent dangerous clots in sepsis patients without increasing their risk of bleeding,” McCarty said. “This could be a game-changer for the treatment of sepsis and help save lives.”
Clinical Implications and Future Directions
The OHSU team’s interdisciplinary approach to the study of sepsis is one of the key factors driving their success. McCarty noted that their work spans from laboratory research to clinical trials, ensuring that discoveries are not only innovative but also applicable to patient care. The collaboration between basic scientists like Lira, who studies the physics of bacterial interactions, and clinicians like Shatzel, who works directly with sepsis patients, makes this research particularly impactful.
As the team continues its studies, they are also focused on securing funding for further research and expanding clinical trials. These trials will test the effectiveness of factor XII-targeting antibodies and explore the broader application of this treatment approach in sepsis patients. The hope is that, with more research and clinical validation, this new treatment strategy could significantly improve the survival rate for patients with sepsis, a disease that kills millions every year.
“The need for new therapies for sepsis is critical. The mortality rate remains shockingly high, and there have been few breakthroughs in decades,” Shatzel said. “Our team is working hard to address this gap. With targeted therapies that can prevent dangerous clots without increasing bleeding, we believe we can make a real difference in the lives of sepsis patients.”
A Collaborative Effort: The OHSU Advantage
The success of this research is not only due to the dedication of the individual researchers but also to the unique collaborative environment at OHSU. The seamless integration of laboratory science, patient care, and clinical trials creates an environment where breakthroughs can happen rapidly. As Shatzel noted, “This program truly spans the gap between lab research and patient care, which is rare in academic settings. We’re able to work from test tubes to animal models to clinical trials, all under one roof.”
McCarty also emphasized the importance of their team’s interdisciplinary approach, highlighting the diverse expertise that contributes to the project’s success. “From physicists to clinicians, each member of our team brings a unique perspective to the table. This collaboration is what makes our breakthroughs possible.”
As the team looks to the future, they remain excited about the potential impact of their research on the treatment of sepsis. Lira put it simply: “There’s still a long way to go, but the possibility of helping patients drives us forward.”
Conclusion
The groundbreaking research from Oregon Health & Science University provides new hope for improving the treatment of sepsis, a condition that continues to claim millions of lives each year. By focusing on the clotting mechanisms triggered by bacterial molecules like LPS, the team has uncovered a promising new therapeutic target in the form of factor XII. With ongoing clinical trials and a commitment to precision medicine, the researchers are optimistic that their work could one day revolutionize sepsis treatment and save countless lives. Their collaborative, interdisciplinary approach exemplifies how combining basic science with patient care can lead to truly transformative advances in medical research.
Reference: André L. Lira et al, The physicochemical properties of lipopolysaccharide chemotypes regulate activation of the contact pathway of blood coagulation, Journal of Biological Chemistry (2024). DOI: 10.1016/j.jbc.2024.108110