A groundbreaking study published in Science by researchers at the National Institutes of Health (NIH) introduces a novel class of antibodies capable of targeting previously unexplored regions of the malaria parasite. This discovery could revolutionize malaria prevention strategies, offering fresh hope in the global fight against one of the deadliest diseases affecting humanity.
Malaria, caused by Plasmodium parasites transmitted through mosquito bites, remains a global health crisis. Despite progress in combating the disease, it continues to claim hundreds of thousands of lives each year, primarily in sub-Saharan Africa. According to the World Health Organization (WHO), malaria caused 263 million infections and 597,000 deaths in 2023, with children being the most vulnerable. The urgent need for innovative and effective interventions has driven extensive research into vaccines, treatments, and antibody-based therapies.
The study focuses on a new class of anti-malarial monoclonal antibodies (mAbs) that target unique regions of the Plasmodium falciparum parasite, the most lethal species of the parasite. These regions are not addressed by current malaria vaccines, making these antibodies a promising addition to the arsenal of tools against the disease. The researchers identified these antibodies by analyzing immune responses in humans exposed to the parasite and evaluating their effectiveness in animal models.
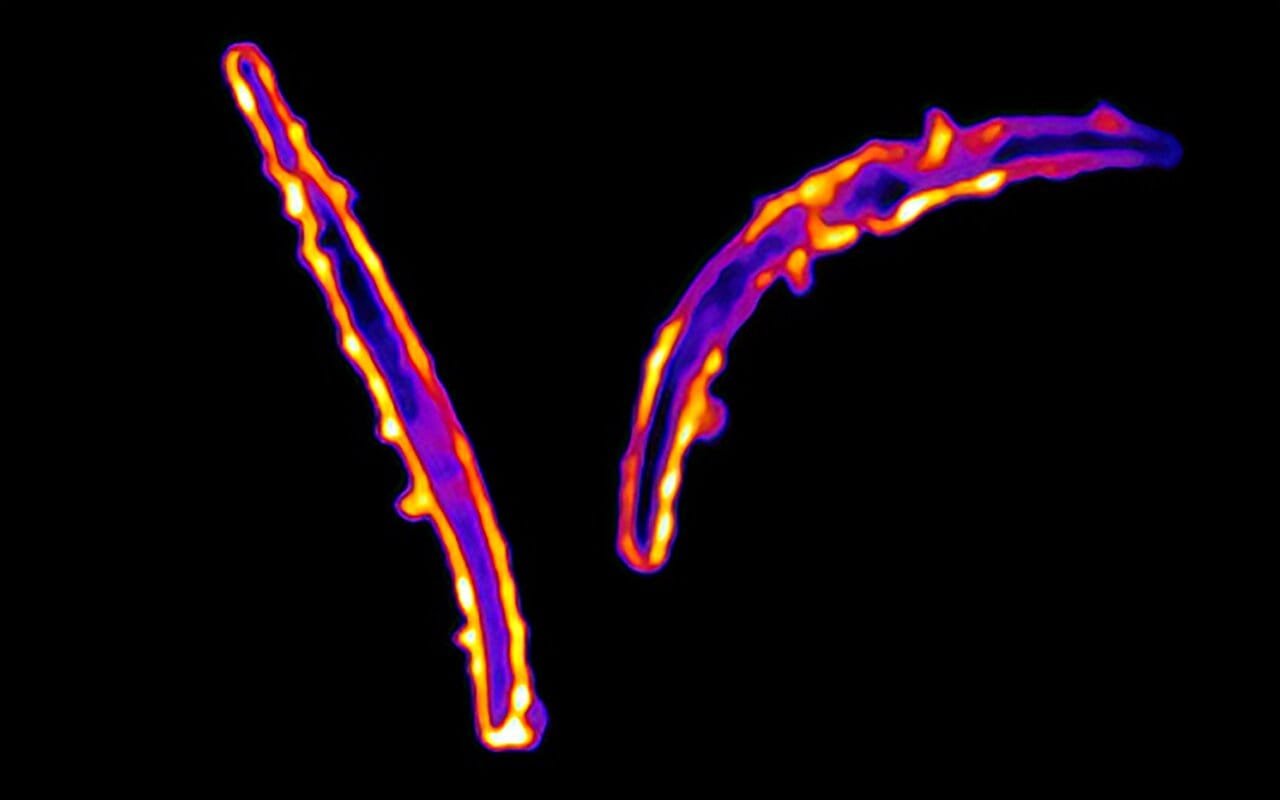
One antibody, designated MAD21-101, demonstrated remarkable potency in protecting mice from P. falciparum infection. Unlike existing vaccines and therapies that focus on the central repeat region of a protein on the parasite’s surface—circumsporozoite protein (PfCSP)—MAD21-101 binds to a newly identified site called pGlu-CSP. This epitope becomes accessible during a critical phase of the parasite’s development, making it an attractive target for immune responses.
The unique properties of this new antibody class present several advantages. Since pGlu-CSP is not included in current malaria vaccines, antibodies targeting this region are unlikely to interfere with vaccine efficacy. This opens the door for co-administration of vaccines and these antibodies, particularly in vulnerable populations such as infants who are not yet vaccinated but remain at high risk of infection.
The findings also underscore the importance of broadening the scope of malaria research to explore less-studied regions of the parasite. Current interventions, including vaccines and mAbs, predominantly target the sporozoite stage of the parasite, specifically the central repeat region of PfCSP. While effective, these approaches have limitations, including strain-specific efficacy and the potential for the parasite to develop resistance.
By identifying and targeting a conserved epitope like pGlu-CSP, the NIH researchers have introduced a potentially universal strategy that could overcome these limitations. This discovery not only enhances our understanding of the parasite’s biology but also lays the foundation for a new generation of countermeasures that could be deployed alongside existing interventions.
The implications of this study extend beyond malaria. The novel approach used to identify these antibodies—analyzing immune responses to whole sporozoites rather than isolated proteins—could be applied to other infectious diseases. This methodology has the potential to uncover new epitopes and antibody classes for pathogens that have thus far evaded effective immune targeting.
The potential for these antibodies to be integrated into current malaria prevention strategies is significant. For instance, they could be administered to at-risk populations during peak transmission seasons or to travelers visiting malaria-endemic regions. Additionally, their ability to complement existing vaccines and therapies offers a flexible and robust approach to malaria control.
Despite the promising findings, the researchers emphasize the need for further investigation. Additional studies are required to confirm the efficacy and safety of these antibodies in humans and to determine the best ways to integrate them into existing malaria prevention programs. Large-scale clinical trials will be essential to assess their potential to reduce malaria transmission and mortality rates in real-world settings.
Moreover, the researchers note that understanding the immune mechanisms triggered by pGlu-CSP could inform the design of next-generation vaccines. By incorporating this epitope into vaccine formulations, it may be possible to create more comprehensive immunizations capable of eliciting a robust and long-lasting protective response.
The discovery of these antibodies represents a significant milestone in malaria research. It highlights the importance of innovation in addressing persistent global health challenges and underscores the potential of cutting-edge science to transform our approach to disease prevention and treatment. With continued investment and collaboration, the fight against malaria could soon enter a new era, marked by more effective, equitable, and sustainable solutions.
As the global community strives to meet ambitious targets for malaria elimination, including those outlined in the WHO’s Global Technical Strategy for Malaria, breakthroughs like this offer renewed hope. By expanding the toolkit available to combat this devastating disease, the novel class of antibodies discovered by NIH researchers could play a pivotal role in reducing the burden of malaria and saving countless lives. The journey from laboratory discovery to clinical application will undoubtedly be complex, but the potential rewards make it an endeavor of the highest importance.
Reference: Cherrelle Dacon et al, Protective antibodies target cryptic epitope unmasked by cleavage of malaria sporozoite protein, Science (2025). DOI: 10.1126/science.adr0510
Think this is important? Spread the knowledge! Share now.