The connection between poor sleep and mental health problems has long intrigued scientists, yet understanding the exact mechanisms behind this link has proven challenging. Researchers at the University of East Anglia (UEA) have now shed new light on the subject, identifying specific deficits in brain regions responsible for keeping unwanted thoughts out of mind as a potential factor. Their findings, published in the Proceedings of the National Academy of Sciences, suggest that sleep deprivation may impair memory control mechanisms, contributing to emotional dysregulation and mental health challenges such as depression and anxiety.
Sleep disturbances are widely recognized as both a symptom and a contributing factor to mental health disorders. Insomnia, sleep apnea, and other issues disrupt the restorative processes of the brain, exacerbating stress, mood disorders, and even severe conditions like post-traumatic stress disorder (PTSD). However, the precise relationship between inadequate sleep and mental health has been elusive until now. This groundbreaking study bridges that gap by exploring the cognitive and neural foundations of memory suppression and its dependence on sleep.
The research team, led by Dr. Marcus Harrington from UEA’s School of Psychology, conducted the study in collaboration with colleagues from the universities of York, Cambridge, Sussex, and Queen’s University in Canada. Their investigation centered on understanding how sleep affects the brain’s ability to suppress unwanted memories—a function critical to emotional regulation and mental health. The study utilized functional neuroimaging to measure activity in brain regions associated with memory control, revealing the detrimental effects of sleep deprivation on these mechanisms.
Dr. Harrington’s work builds upon the premise that unwanted memories, particularly those tied to unpleasant or traumatic experiences, can intrude into consciousness, often in response to external triggers. For most people, these intrusions are fleeting and manageable. However, for individuals with mental health disorders, such memories can become persistent, vivid, and deeply distressing. Conditions such as depression, anxiety, and PTSD frequently involve intrusive memories that disrupt daily functioning and intensify emotional struggles.
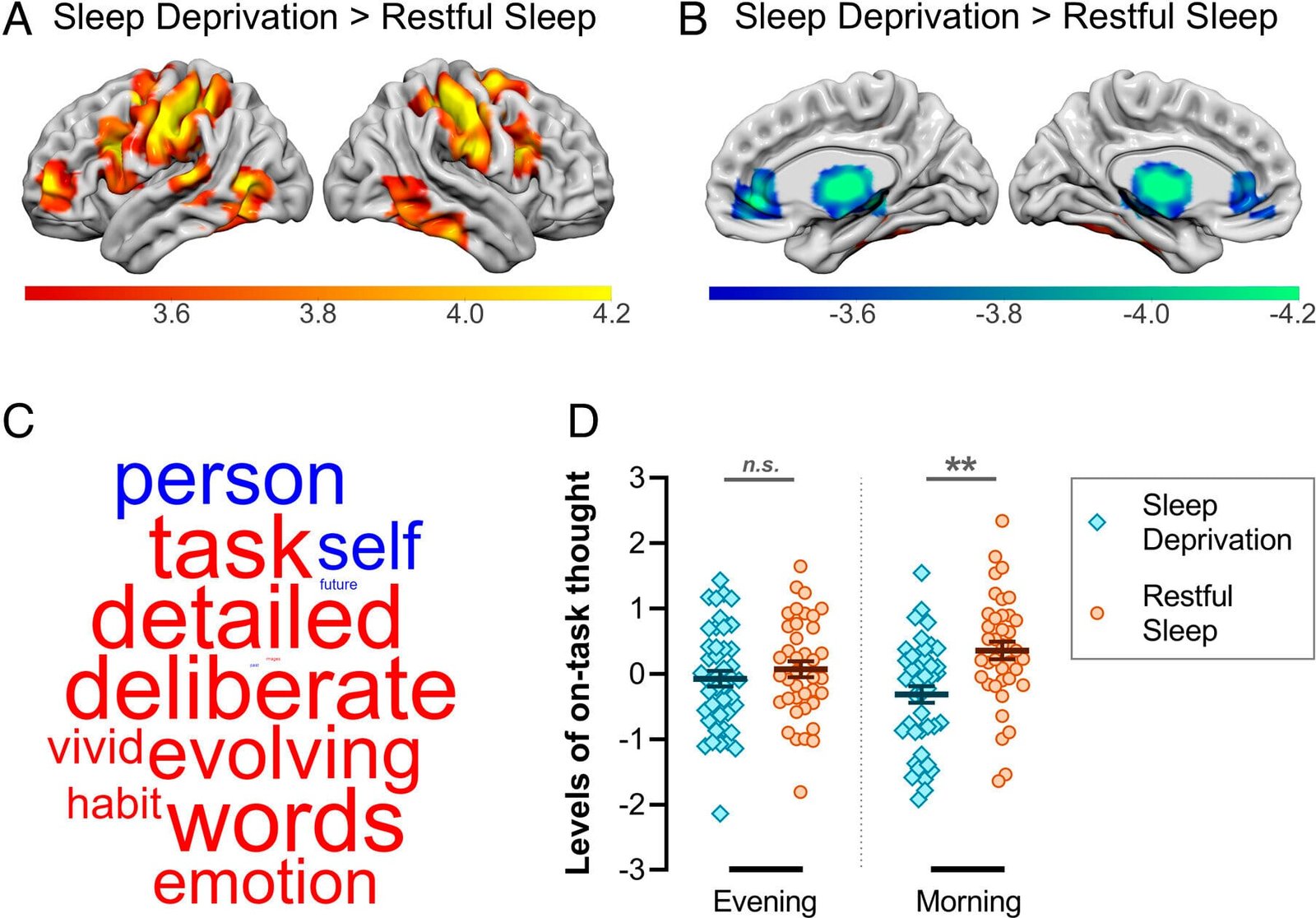
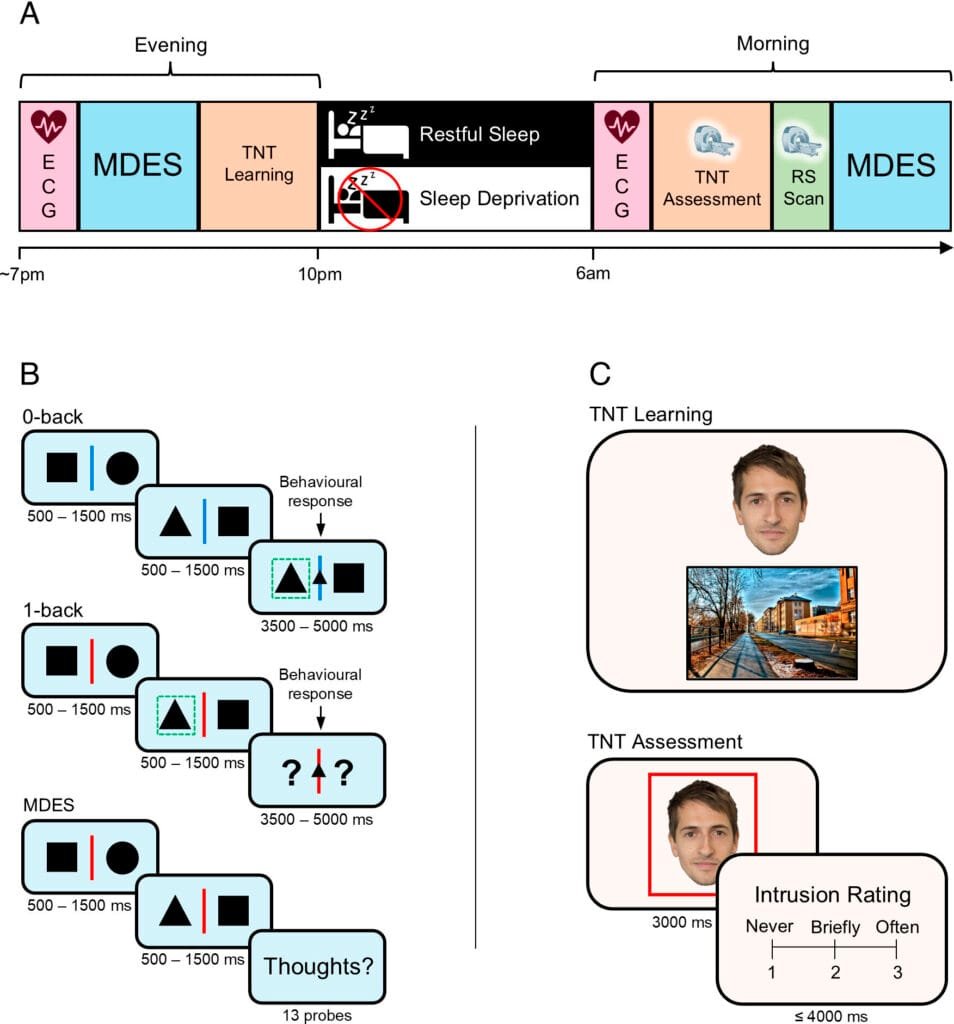
In the study, 85 healthy adults participated in tasks that required suppressing unwanted memories while their brain activity was monitored using functional MRI. Half of the participants experienced a full night of restful sleep in a controlled laboratory environment, while the other half were required to stay awake throughout the night. The researchers compared the neural responses between the two groups during memory suppression tasks.
Their findings were striking. Participants who slept showed increased activation in the right dorsolateral prefrontal cortex—a critical brain region responsible for managing thoughts, emotions, and behaviors. Conversely, those deprived of sleep exhibited diminished activation in this area. At the same time, the rested participants demonstrated reduced activity in the hippocampus, the brain region associated with retrieving memories. This suggests that sleep bolsters the brain’s ability to regulate memory retrieval, preventing unwanted memories from entering conscious thought.
One particularly intriguing discovery was the role of rapid eye movement (REM) sleep in this process. REM sleep is a distinct phase of the sleep cycle characterized by vivid dreams and significant brain activity. Among the well-rested participants, those who spent more time in REM sleep were better able to engage the dorsolateral prefrontal cortex during memory suppression tasks. This indicates that REM sleep plays a crucial role in rejuvenating the brain’s control mechanisms, enhancing the ability to suppress intrusive memories.
The implications of these findings are profound. Memory control failures, exacerbated by sleep loss, may underlie many of the emotional and cognitive symptoms observed in mental health disorders. Dr. Harrington noted that understanding the mechanisms that lead to such failures is critical to improving emotional well-being and addressing the global mental health crisis. Intrusive memories are a central feature of many disorders, and identifying the role of sleep in mitigating their impact opens new avenues for treatment and prevention.
Sleep’s role in maintaining mental health is complex but increasingly clear. It is during sleep that the brain consolidates memories, processes emotions, and rejuvenates neural pathways. Disrupting these processes impairs emotional regulation, decision-making, and cognitive function, all of which are essential to maintaining mental health. The findings of this study reinforce the idea that prioritizing sleep is not just beneficial for physical health but is also a cornerstone of psychological well-being.
In addition to its contributions to understanding the link between sleep and mental health, this research has broader implications for the treatment and prevention of mental illnesses. By highlighting the importance of REM sleep in restoring memory control mechanisms, the study points to potential therapeutic strategies aimed at enhancing sleep quality. Cognitive-behavioral therapy for insomnia (CBT-I), pharmacological interventions, and lifestyle changes could all be leveraged to improve sleep and, by extension, emotional health.
Furthermore, these insights may inform targeted therapies for specific mental health conditions characterized by intrusive memories, such as PTSD. Treatments designed to enhance prefrontal cortex function or to extend REM sleep could help patients better manage distressing memories. Understanding the neural pathways involved in memory suppression also opens doors for non-invasive brain stimulation techniques, such as transcranial magnetic stimulation (TMS), as a potential adjunct to traditional therapies.
On a societal level, this research underscores the importance of addressing sleep disorders as part of mental health care. Sleep disturbances are often dismissed as secondary symptoms of mental illness, rather than as primary issues needing intervention. However, the bidirectional relationship between sleep and mental health suggests that improving sleep quality could yield significant benefits for mental well-being, reducing the burden of mental illness globally.
Reference: Marcus O. Harrington et al, Memory control deficits in the sleep-deprived human brain, Proceedings of the National Academy of Sciences (2024). DOI: 10.1073/pnas.2400743122
Think this is important? Spread the knowledge! Share now.