The rise of antibiotic-resistant bacteria has become one of the most pressing health concerns of the 21st century, with new research from Northern Arizona University (NAU) highlighting the catastrophic potential of these superbugs. According to the study, which was published in Communications Medicine, the increase in multidrug-resistant bacteria could lead to a dramatic surge in infection-related deaths worldwide. This grim outlook serves as a stark warning: it’s not a question of whether antibiotic resistance will spiral out of control, but rather when it will do so.
Benjamin Koch, the lead author and senior research scientist at NAU’s Center for Ecosystem Science and Society (Ecoss), emphasized that the situation could evolve rapidly once bacteria become resistant to all known antibiotics—a condition known as pan-resistance. Koch explained that while multidrug-resistant bacteria are already a significant problem, pan-resistance could cause a sudden, catastrophic rise in public health impacts, surpassing anything currently anticipated. This shift would not be gradual but could unfold with alarming speed.
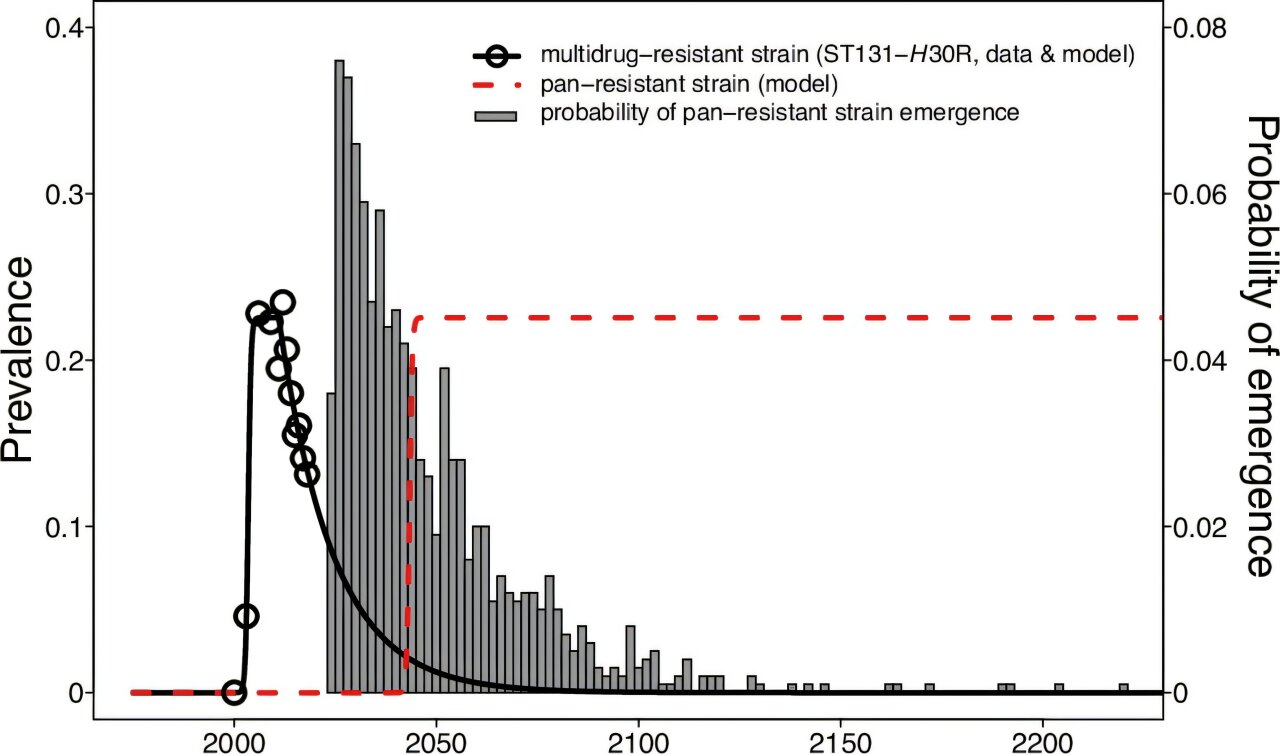
The research team, including Ecoss director Bruce Hungate, Regents’ Professor of Biology, along with experts from the Milken Institute School of Public Health at George Washington University and the University of Minnesota, aimed to model the potential consequences of a pan-resistant strain of bacteria. The study specifically focused on sepsis deaths in the United States, using long-term data to estimate the likely impact of a hypothetical strain of pan-resistant E. coli. The findings were sobering: if such a strain were to emerge, the rate of sepsis deaths could increase by 18 to 46 times just five years after its introduction.
Although this pan-resistant strain does not yet exist, the rapid pace at which bacteria are evolving and gaining resistance to multiple antibiotics suggests it is only a matter of time before such a strain appears. Koch and his colleagues caution that while the exact timing is impossible to predict—ranging from just a year to perhaps a century—the inevitability of pan-resistance is clear.
The global implications of pan-resistant bacteria are profound. Historically, people in high-income countries have had the advantage of access to advanced medical care and a wide variety of antibiotics. This access has enabled healthcare systems to manage infections that would otherwise be fatal. However, pan-resistance undermines these advantages, as no antibiotics would be effective against resistant pathogens. As a result, even individuals in wealthier nations would be at risk, and mortality rates from previously treatable infections would rise dramatically. The global nature of the problem means that people from all walks of life, regardless of socioeconomic status, would be impacted.
The bad news doesn’t end there. The threat of pan-resistant bacteria is exacerbated by the overuse and misuse of antibiotics in both human and veterinary medicine. The use of antibiotics in food-animal production, where they are often employed to promote growth rather than to treat illness, also contributes to the development of resistance. The proliferation of antibiotic-resistant pathogens is directly linked to these practices, and without a concerted global effort to curb their use, the emergence of pan-resistant bacteria is all but guaranteed.
However, all hope is not lost. The study highlights several measures that can be taken to mitigate the risk and slow the spread of antibiotic resistance. Governments, industries, and individuals each have a role to play in combating this growing threat. For governments, strengthening policies around the safe use of antibiotics in both healthcare and agriculture is crucial. This includes implementing stricter regulations on antibiotic use in food-animal production and enforcing guidelines for proper antibiotic prescribing in human medicine. Additionally, there is a pressing need to incentivize the development of new antibiotics. In recent years, the rate at which new antibiotics are being developed has slowed to a near halt, largely due to economic and regulatory challenges. Governments and private companies must work together to overcome these barriers and accelerate the discovery of new treatments.
On an individual level, there are steps that everyone can take to reduce the spread of antibiotic-resistant bacteria. First and foremost, people should use antibiotics only when necessary and always as prescribed by a healthcare provider. Misuse, such as taking antibiotics for viral infections like the flu, contributes significantly to the development of resistance. Individuals should also advocate for policies that strengthen antibiotic stewardship—the practice of ensuring that antibiotics are used only when absolutely necessary and in the correct manner. Supporting research into new antibiotics is another critical action, as the development of novel treatments will be essential in the fight against pan-resistance.
Researchers also point to the importance of monitoring the emergence and spread of antibiotic resistance through new technologies. Surveillance systems that track resistance patterns globally could help identify threats early and guide the development of strategies to combat them. These technologies could provide valuable data for public health authorities, enabling them to respond more effectively to outbreaks of resistant infections.
The study’s authors conclude with a stark reminder: we must urgently address the forces that promote the evolution and dissemination of antibiotic-resistant pathogens. This includes improving antibiotic stewardship in both human and veterinary medicine, as well as in food-animal production. Failure to do so will likely lead to a future where the most basic infections become deadly once again, a scenario that could reverse decades of progress in public health and medicine.
Reference: Benjamin J. Koch et al, Predicting sepsis mortality into an era of pandrug-resistant E. coli through modeling, Communications Medicine (2024). DOI: 10.1038/s43856-024-00693-7