In late 2019, a mysterious virus emerged in Wuhan, China, igniting what would soon become the most devastating pandemic in a century. Within weeks, scientists around the world sprang into action, not only to understand the virus but also to develop a vaccine to stop its spread. What followed was a scientific revolution—a turning point in the history of medicine, fueled by a molecule once considered too unstable and too obscure for therapeutic use: RNA.
Messenger RNA, or mRNA, leapt from textbooks into the limelight, becoming the cornerstone of the world’s first highly effective COVID-19 vaccines. The success of the mRNA-based vaccines developed by Pfizer-BioNTech and Moderna marked a milestone in medical science. These vaccines not only helped contain the pandemic but also opened new frontiers in vaccine development and disease prevention.
This article explores the fascinating story of RNA and its unprecedented role in the fight against COVID-19. From the molecular structure of RNA to the history of its scientific development, from how mRNA vaccines work to the promise they hold for future therapies—this is the story of how a once-overlooked strand of genetic material became humanity’s greatest weapon in a global crisis.
Understanding RNA: The Silent Messenger of Life
RNA, or ribonucleic acid, is one of the most fundamental molecules of life. Alongside DNA and proteins, it forms the central dogma of molecular biology: DNA makes RNA, and RNA makes protein. While DNA serves as the long-term storage of genetic information, RNA acts as the working copy, a messenger that carries instructions from the nucleus to the ribosomes—the molecular machines that build proteins.
RNA is a single-stranded molecule composed of nucleotides, each containing a sugar (ribose), a phosphate group, and one of four nitrogenous bases: adenine (A), cytosine (C), guanine (G), or uracil (U)—which replaces thymine (T) found in DNA. Its structure makes it more versatile but also more fragile than DNA. This fragility was once considered a major obstacle for its use in medicine. Yet, as we now know, this very feature turned out to be a benefit for vaccine design.
There are several types of RNA, but the one central to COVID-19 vaccines is messenger RNA (mRNA). This is the form that carries genetic instructions from DNA to direct protein synthesis. In a sense, mRNA is the blueprint for life in motion—a script that tells cells what proteins to make and when to make them.
A Brief History of mRNA Science: From Curiosity to Cure
The path from RNA discovery to RNA vaccine has been a long and winding one. RNA was first identified in the 1930s, but its role as a messenger molecule wasn’t fully understood until the 1960s. The initial excitement around RNA as a potential therapeutic tool was tempered by its inherent instability—it degrades rapidly in the body and is easily destroyed by enzymes called RNases.
Still, visionary scientists persisted. In the 1980s and 1990s, researchers began experimenting with synthetic mRNA as a way to express proteins in cells, a crucial step toward therapeutic applications. However, challenges remained. The immune system would often react to the introduced mRNA as if it were a dangerous virus. Moreover, the mRNA itself was unstable, breaking down before it could do its job.
A major breakthrough came in the early 2000s, thanks in large part to the work of scientists like Katalin Karikó and Drew Weissman. They discovered that modifying one of the nucleosides in the RNA molecule—specifically replacing uridine with a synthetic analog—could dramatically reduce its immunogenicity and improve its stability. This opened the door to safe and effective mRNA therapies, although the world wouldn’t recognize the value of their work until much later.
The SARS-CoV-2 Virus: Understanding the Enemy
To understand how mRNA vaccines work, we must first understand the virus they were designed to fight. SARS-CoV-2, the virus that causes COVID-19, is a member of the coronavirus family—a group of viruses known for their crown-like appearance under the microscope. Its genetic material is made of RNA, and it primarily infects cells in the respiratory tract.
The virus’s most notorious feature is its spike protein, a surface molecule that allows it to latch onto human cells via the ACE2 receptor. Once attached, the virus fuses with the cell membrane and injects its genetic material, hijacking the cell’s machinery to produce more copies of itself.
Because the spike protein plays such a critical role in viral entry, it became the prime target for vaccine developers. If the immune system could recognize and neutralize the spike protein, it could stop the virus before it ever gained a foothold in the body.
How mRNA Vaccines Work: Programming the Immune System
Traditional vaccines use weakened or inactivated viruses, or pieces of viral proteins, to train the immune system. mRNA vaccines, however, take a radically different approach. Instead of injecting a piece of the virus, scientists inject the genetic instructions for making a harmless version of the viral spike protein. These instructions come in the form of synthetic mRNA.
Once inside the body, the mRNA is absorbed by immune cells, particularly dendritic cells and macrophages. These cells read the mRNA and begin producing the spike protein as if it were their own. The newly made spike protein is then displayed on the surface of these cells or released into the body, where it triggers an immune response.
Importantly, the immune system sees the spike protein as foreign and starts producing antibodies and activating T cells to destroy cells that display it. The result is immunological memory—a rapid and targeted response if the person later encounters the actual virus.
The mRNA in the vaccine does not enter the nucleus of the cell and cannot alter DNA. It is broken down naturally within a matter of hours or days, leaving behind only the immune memory that provides protection.
The Pfizer-BioNTech and Moderna Vaccines: A Tale of Two Breakthroughs
The two mRNA vaccines that have become household names—Pfizer-BioNTech’s BNT162b2 and Moderna’s mRNA-1273—are strikingly similar in design but differ in formulation and storage requirements.
Both vaccines use lipid nanoparticles (LNPs) to encase and protect the fragile mRNA molecules. These LNPs help the mRNA enter cells by fusing with the cell membrane. Once inside, the mRNA is translated into the spike protein, and the immune system responds.
Pfizer-BioNTech’s vaccine was the first to receive emergency use authorization in multiple countries. Moderna’s followed closely behind. Both vaccines demonstrated remarkable efficacy—over 90%—in preventing symptomatic COVID-19 in clinical trials. This was far higher than many had hoped and marked a turning point in the fight against the pandemic.
These vaccines also proved to be adaptable. As new variants of SARS-CoV-2 emerged, scientists were able to tweak the mRNA code to better match the mutated spike proteins—showcasing the flexibility and speed of mRNA technology.
Safety and Side Effects: Balancing Benefit and Risk
As with any vaccine, mRNA-based vaccines come with some side effects. The most common are mild to moderate and include pain at the injection site, fatigue, headache, chills, and fever. These symptoms usually resolve within a day or two and are signs that the immune system is responding.
In rare cases, more serious adverse events have been reported, such as myocarditis (inflammation of the heart) in younger males and anaphylaxis in individuals with certain allergies. However, these risks are significantly outweighed by the benefits of vaccination, especially in preventing severe illness, hospitalization, and death due to COVID-19.
Importantly, millions of doses have been administered worldwide, and the safety profile of mRNA vaccines continues to be monitored and evaluated through ongoing surveillance systems and studies.
Debunking the Myths: mRNA Does Not Alter Your DNA
A major concern among some people is the misconception that mRNA vaccines can change one’s genetic code. This is biologically implausible. mRNA vaccines do not enter the cell nucleus, where DNA is stored, and they do not integrate into the genome. The mRNA is simply a temporary set of instructions that directs protein production and is then destroyed.
This fear reflects a broader challenge in public health communication—how to convey the science of novel technologies in ways that are transparent, accurate, and accessible. Addressing misinformation with empathy and evidence is essential to building trust and achieving widespread vaccine acceptance.
The Logistics of mRNA Vaccines: Challenges and Triumphs
Creating an mRNA vaccine is only part of the battle—delivering it to billions of people around the world is another. One of the biggest challenges has been storage and transportation. mRNA is highly unstable and requires ultracold storage to remain viable. The Pfizer-BioNTech vaccine originally required temperatures of -70°C, while Moderna’s could be stored at -20°C.
These requirements posed logistical hurdles, especially in low-resource settings. Over time, improvements in formulation and stability have allowed for more flexible storage conditions, but the cold chain remains a critical component of mRNA vaccine distribution.
Despite these obstacles, the scale of the vaccine rollout has been unprecedented. Within a year of the virus’s emergence, billions of doses were produced, shipped, and administered—an extraordinary feat of global collaboration.
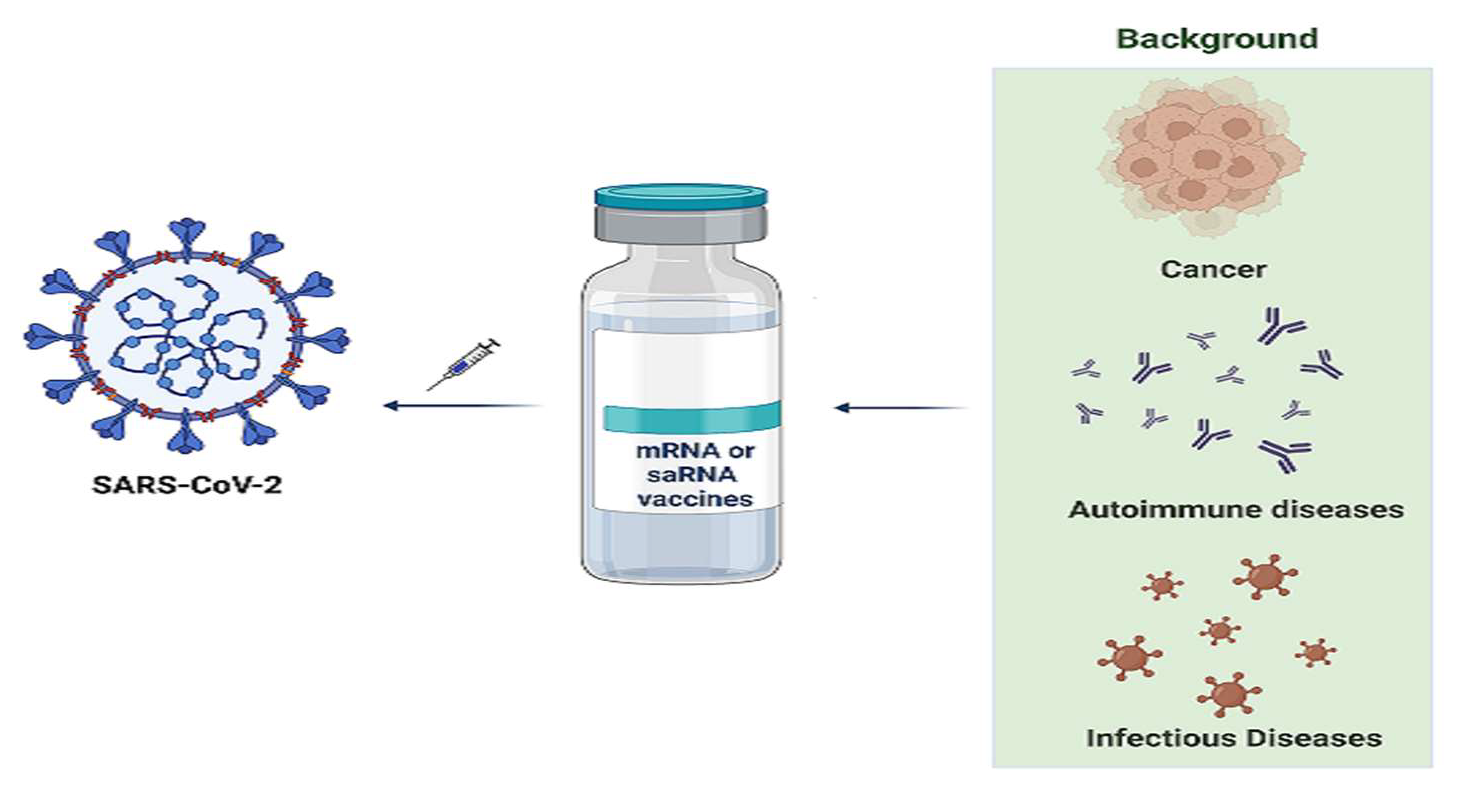
The Future of mRNA Vaccines: Beyond COVID-19
The success of mRNA vaccines against COVID-19 has ignited a wave of research into their use for other infectious diseases and even non-infectious conditions. mRNA platforms are now being developed for influenza, HIV, Zika, rabies, and more. Some researchers are exploring pan-coronavirus vaccines that could provide immunity against multiple coronaviruses, including future strains.
Beyond infectious diseases, mRNA is being tested in cancer immunotherapy, where personalized vaccines can teach the immune system to recognize and destroy tumor cells. There’s also growing interest in mRNA for autoimmune diseases, allergies, and genetic disorders—potentially offering new treatments for conditions that were once considered incurable.
What makes mRNA so promising is its adaptability. Once the platform is established, new vaccines can be designed and manufactured quickly—something that could be vital in future pandemics.
Conclusion: A Scientific Milestone Written in RNA
The COVID-19 pandemic has changed the world in countless ways, but one of its most profound legacies may be the rise of RNA as a central player in medicine. What was once a fragile molecule confined to the laboratory has become a global hero—powering vaccines that saved millions of lives and redefined what is possible in modern science.
The journey of mRNA, from the periphery of molecular biology to the forefront of global health, is a story of perseverance, ingenuity, and hope. It reminds us that the tiniest molecules can have the biggest impact—and that when science and humanity come together, we can rewrite the future.