A team of scientists from the University of Massachusetts Amherst and Ernest Pharmaceuticals has made significant strides in developing a groundbreaking cancer treatment that could reshape the way we treat tumors. The innovative technology, BacID, leverages a unique bacterial therapy to directly deliver cancer-fighting drugs to tumors in a highly targeted and non-toxic manner. This approach holds the potential to revolutionize cancer treatment, offering a much safer and more effective alternative to conventional therapies such as chemotherapy. The new findings mark a major milestone for a technology that could one day treat highly lethal cancers, including liver, ovarian, and metastatic breast cancers.
The Development of BacID
The researchers have been working on BacID for over a decade, and the work is beginning to bear fruit. Led by Neil Forbes, a professor of chemical engineering at UMass Amherst, and Vishnu Raman, the senior and lead authors of the study published in Molecular Therapy, the breakthrough is one of the latest in a series of promising bacterial cancer treatments. This technology relies on genetically engineered bacteria, particularly strains of Salmonella, to deliver drugs directly into cancer cells, bypassing healthy tissues entirely. By delivering a much higher concentration of treatment directly to the tumors, the system offers potentially better efficacy and fewer side effects than conventional chemotherapy, which often affects healthy cells and causes debilitating side effects.
“What we’re trying to do is unlock the potential to treat late-stage cancers,” says Raman, who completed his Ph.D. in Forbes’ lab at the UMass Institute for Applied Life Sciences (IALS). One of the core principles of this treatment is that bacteria have a natural ability to “home in” on tumors, an intriguing characteristic that allows this therapy to be incredibly targeted.
BacID’s Uniqueness: Targeting Tumors Safely
The new bacterial treatment works by using genetically engineered Salmonella to invade tumors once inside the body. These bacteria are engineered to be non-toxic and safe for human use, a critical improvement over earlier generations of bacterial therapies that posed risks to healthy tissue. The key feature of this new strain is that it can be easily controlled, allowing the researchers to precisely time when and where the bacteria deliver their cancer-killing payload.
Bacteria, particularly Salmonella, have long been known to have a natural affinity for tumors, often accumulating in tumor tissues due to the microenvironment created by tumors themselves. These bacteria are particularly efficient at growing in tumors because of their ability to rapidly proliferate in the oxygen-poor and nutrient-rich environment present in cancerous tissues. Once inside a tumor, the bacteria grow exponentially, which allows the treatment to deliver far more therapeutic agent than could be achieved through conventional methods. By engineering bacteria with a highly controlled release mechanism, the team was able to significantly improve the safety and targeting of the treatment.
“What we’re aiming to do is drastically reduce the harsh side effects that are often seen with chemotherapy, as well as the off-target effects where healthy organs might suffer unintended harm,” explains Forbes. By using bacteria that home to tumors and then deliver the treatment directly to cancer cells, the platform potentially eliminates much of the systemic toxicity that is commonly associated with chemotherapy and other conventional treatments.
Advances in Genetic Engineering for Safety and Precision
One of the biggest challenges with this type of treatment is ensuring that the bacteria do not attack healthy cells or enter other tissues before being activated in the target area. In earlier strains of bacterial therapy, this problem was common. The first-generation bacteria simply relied on their natural ability to locate tumors, without any mechanism for controlling when or how they would invade the cells.
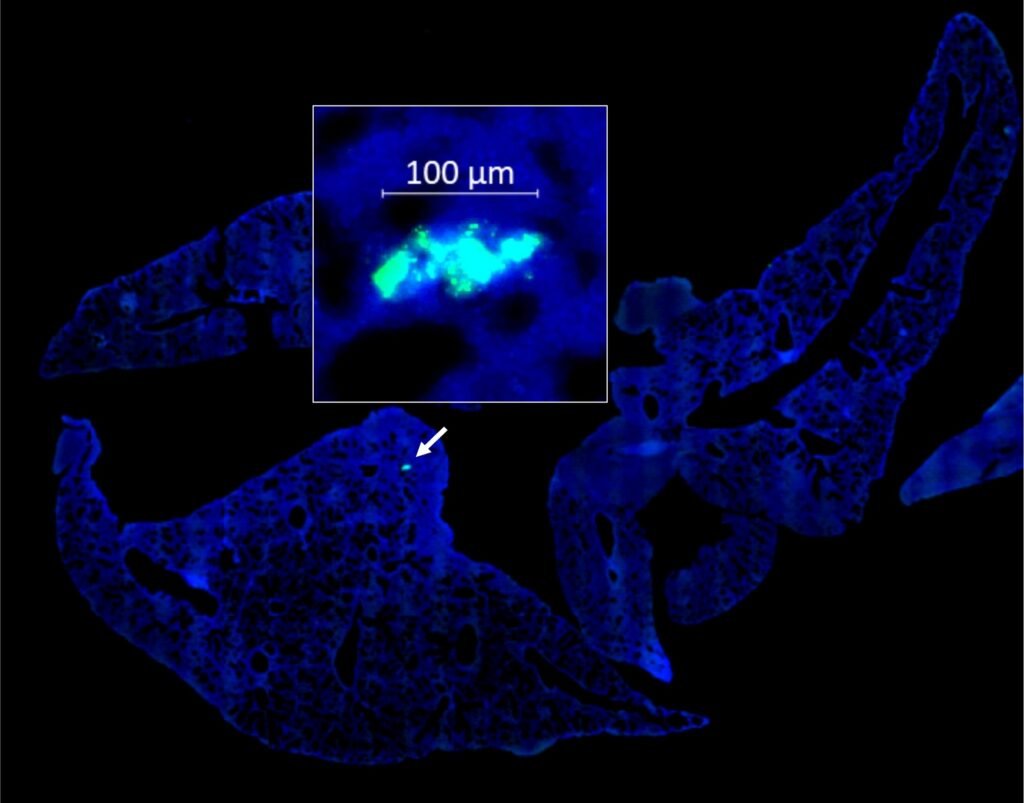
The new strain of Salmonella developed by the team, however, incorporates genetic modifications that provide more control. This “third-generation” strain allows for a precision-triggered response that prevents unintended tissue damage. A major breakthrough occurred when the researchers identified that Salmonella‘s flagella — the tail-like appendages responsible for bacterial movement — were the key to allowing the bacteria to penetrate cancer cells. By engineering a genetic switch that controls the production of flagella, the bacteria remain dormant until they are activated by a simple, over-the-counter dose of aspirin, which contains salicylic acid.
“When a patient takes aspirin, salicylic acid enters the bloodstream and activates the bacteria, causing them to produce flagella. This is the trigger for the bacteria to invade cancer cells,” explains Raman. This innovation allows researchers to prevent the bacteria from entering non-cancerous cells, enhancing safety and minimizing the risks of off-target invasion.
The bacteria used in BacID are also engineered to include a “suicide circuit.” Once inside a cancer cell, the bacteria rupture and release the cancer-fighting drug they carry. This mechanism helps deliver the drug directly to the tumor cells while ensuring that the bacteria do not live long enough to affect healthy tissue.
How BacID Works: A Step-by-Step Process
In pre-clinical studies, the team demonstrated that when the bacterial strain is injected intravenously into a subject — typically a mouse model in these initial stages — it disperses throughout the body. The immune system quickly clears the bacteria from healthy tissues within the first two days, but the bacteria continue to grow and proliferate exponentially in tumor tissues. Once this happens, the patient is given an aspirin dose, which acts as a trigger to activate the bacteria and start the delivery process.
“When patients receive this treatment, they have the infusion and then a few days later take an oral dose of aspirin at home,” says Raman. This simple and patient-friendly method is one of the major advantages of the BacID system. By integrating a common over-the-counter drug like aspirin into the treatment, the system enhances its accessibility and ease of use, making it far more feasible and less disruptive than traditional therapies that require lengthy hospital visits or complex administration schedules.
The Promise of BacID for Treating High-Mortality Cancers
One of the most compelling aspects of BacID is its potential for treating cancers that are traditionally very difficult to manage and are often diagnosed at later stages when other therapies are no longer effective. Cancers such as metastatic breast cancer, ovarian cancer, and liver cancer can be especially aggressive, and they often have poor survival rates. The development of a more effective and targeted treatment holds tremendous promise for improving outcomes for patients with these difficult-to-treat diseases.
“With BacID, we believe we can safely and effectively target these late-stage cancers,” says Forbes. “Unlike traditional cancer treatments, which are less effective at later stages and come with significant side effects, BacID offers a solution that is both more powerful and safer.”
A Growing Field: The Future of Microbial-Based Cancer Therapy
The work of Raman, Forbes, and the team has put them at the forefront of a rapidly growing field — microbial-based cancer therapy. This exciting area of research is still in its early stages, but it shows significant promise in offering more targeted, effective, and safer treatments for cancer patients. The team is now focused on preparing the BacID technology for clinical trials, with plans to start working with cancer patients by 2027. Clinical trials will be an essential step toward regulatory approval and the eventual introduction of this technology as a treatment option.
“We’ve seen considerable growth and excitement in microbial-based cancer treatment, and we’re excited to lead the charge in this rapidly evolving field,” says Raman. The team is now working diligently to get the necessary regulatory approvals to start clinical trials, which will represent a critical step in bringing BacID closer to becoming a reality for cancer patients.
Conclusion
BacID is a remarkable innovation in cancer treatment, providing a non-toxic, bacteria-based therapy that directly delivers cancer-killing drugs into tumors. By harnessing the natural properties of Salmonella and engineering them to target tumors in a controlled, patient-friendly manner, this technology has the potential to revolutionize the treatment of high-mortality cancers like liver, ovarian, and metastatic breast cancer. As research progresses and clinical trials begin, BacID may offer hope to many cancer patients who are currently limited by the side effects and ineffectiveness of traditional therapies. The innovative work being done at UMass Amherst and Ernest Pharmaceuticals is pushing the boundaries of what’s possible in cancer treatment, offering a promising glimpse of a future where cancer can be treated more safely and effectively.
Reference: Vishnu Raman et al, Controlling intracellular protein delivery, tumor colonization and tissue distribution using the master regulator flhDC in a clinically relevant ΔsseJ Salmonella strain, Molecular Therapy (2024). DOI: 10.1016/j.ymthe.2024.12.038
Behind every word on this website is a team pouring heart and soul into bringing you real, unbiased science—without the backing of big corporations, without financial support.
When you share, you’re doing more than spreading knowledge.
You’re standing for truth in a world full of noise. You’re empowering discovery. You’re lifting up independent voices that refuse to be silenced.
If this story touched you, don’t keep it to yourself.
Share it. Because the truth matters. Because progress matters. Because together, we can make a difference.
Your share is more than just a click—it’s a way to help us keep going.
