Imagine a battlefield so small you can’t see it with the naked eye, yet upon it the fate of millions of lives has been decided. This battlefield exists within our bodies, on our skin, and in the world around us—every second of every day. It is the site of an ancient and ongoing war: the struggle between microscopic invaders called bacteria and one of humankind’s greatest weapons—antibiotics.
These drugs have transformed medicine, turning once-deadly infections into treatable inconveniences. The discovery of antibiotics not only extended human life but revolutionized surgery, childbirth, and even cancer treatment. Yet this war is not one-sided. Bacteria are cunning, adaptive, and relentless foes. The more we learn about antibiotics, the more we realize that we are locked in a dynamic and evolving conflict, one that demands ingenuity, caution, and a deep understanding of the enemy.
This article takes you deep into the science of antibiotics. We’ll uncover how they work, how they are made, how bacteria fight back, and why the stakes in this molecular war are higher now than ever before. From the invention of penicillin to the terrifying rise of drug-resistant superbugs, this is the fascinating story of the invisible battle for health and survival.
Understanding the Enemy: What Are Bacteria?
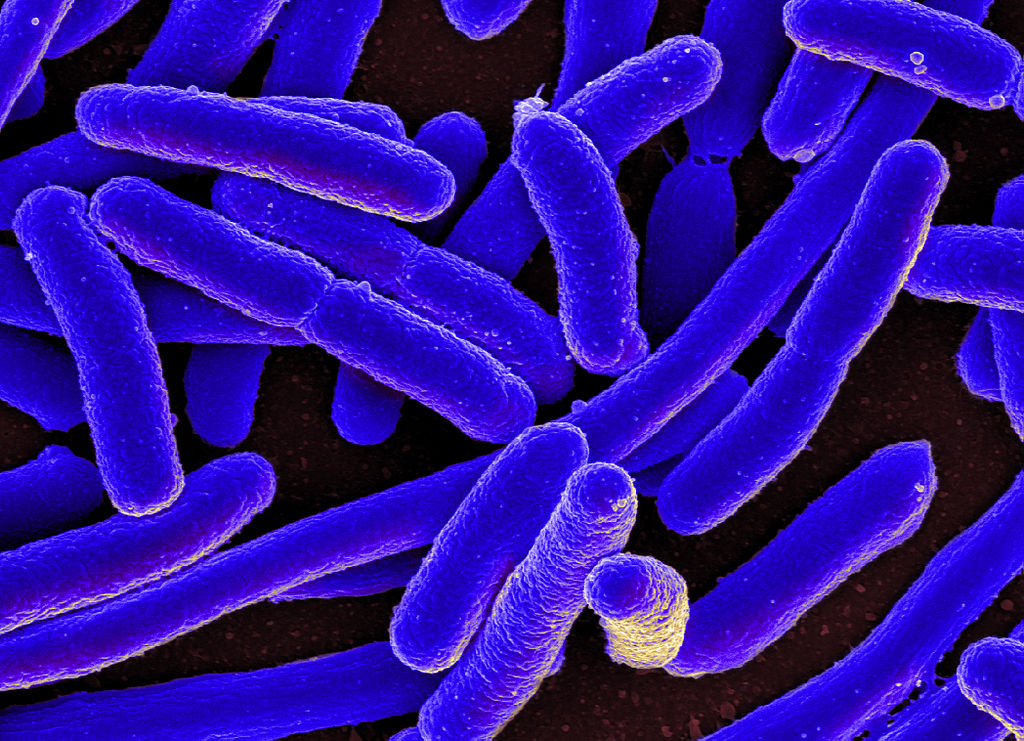
Before diving into antibiotics, we need to understand the organisms they target. Bacteria are single-celled microorganisms that belong to their own domain of life. They’re found virtually everywhere: in soil, oceans, hot springs, and even inside our bodies. In fact, your body contains more bacterial cells than human cells—most of them beneficial or harmless.
Bacteria reproduce rapidly, often doubling in number every 20 minutes under optimal conditions. They have a simple structure, with no nucleus or organelles, but they are far from primitive. Their genetic flexibility and ability to adapt make them formidable. Some live communally in colonies, sharing nutrients and even genetic material. Others are pathogens—disease-causing agents capable of infecting humans, animals, and plants.
These pathogenic bacteria are the targets of antibiotics. But how do these drugs distinguish between harmful bacteria and the cells of our own bodies? The answer lies in the unique features of bacterial cells.
The Discovery of Antibiotics: A Chance Encounter
The story of antibiotics began with an accident. In 1928, Scottish scientist Alexander Fleming returned to his lab after a vacation and noticed that a mold, Penicillium notatum, had contaminated one of his petri dishes. Around the mold was a clear zone where bacteria had been killed. Fleming had discovered penicillin, the world’s first true antibiotic.
Penicillin would not be mass-produced until the 1940s, when it was used to treat wounded soldiers in World War II. Its success was spectacular. Infections that once meant certain death were now curable. Scientists quickly discovered more antibiotics, ushering in a golden age of antimicrobial discovery. Streptomycin, tetracycline, and erythromycin followed, each working in a slightly different way to disable or destroy bacteria.
But what is it that these drugs actually do at the molecular level?
How Antibiotics Kill or Stop Bacteria
Antibiotics work by targeting specific structures or functions in bacterial cells that human cells do not have. This selectivity allows antibiotics to eliminate bacteria without harming the host. There are several main strategies antibiotics use:
Inhibiting Cell Wall Synthesis
One of the most common targets is the bacterial cell wall, made primarily of a molecule called peptidoglycan. This rigid structure protects the bacterial cell from bursting due to osmotic pressure. Human cells lack a cell wall, making this an ideal target.
Penicillin and its relatives—called beta-lactam antibiotics—block the enzymes that bacteria use to build their cell wall. Without a functioning wall, bacteria swell and burst. Other drugs, like vancomycin, bind directly to peptidoglycan components and prevent their assembly.
Disrupting Protein Synthesis
Bacteria build proteins using structures called ribosomes. While human cells also have ribosomes, bacterial ribosomes are different in shape and composition. Antibiotics like tetracycline, erythromycin, and chloramphenicol attach to these bacterial ribosomes and stop them from making essential proteins. Without proteins, bacteria cannot grow or survive.
Interfering with DNA or RNA Synthesis
Other antibiotics disrupt the process of copying or reading genetic information. Quinolones, such as ciprofloxacin, interfere with enzymes that help bacteria untangle their DNA during replication. Rifampin binds to RNA polymerase, blocking transcription and stopping the bacteria from making RNA.
Damaging Cell Membranes
Some antibiotics, like polymyxins, punch holes in the bacterial cell membrane. This causes the contents of the cell to leak out, quickly killing the bacteria. Because cell membranes are somewhat similar between bacteria and humans, these antibiotics are often used cautiously due to potential toxicity.
Blocking Metabolic Pathways
Sulfonamides and trimethoprim inhibit enzymes involved in folate synthesis, a vitamin pathway essential for bacterial survival but unnecessary for humans, who obtain folate from their diet. These drugs are often used in combination to increase their effectiveness.
Each of these mechanisms strikes a vital process in bacterial cells, crippling them with surgical precision. But the story doesn’t end there. Bacteria, like all living things, fight back.
The Rise of Resistance: Bacteria Strike Back
If antibiotics are the swords in this molecular war, then antibiotic resistance is the armor worn by bacteria. Resistance can arise in many ways: through random mutations, through gene exchange between bacteria, or even by activation of previously dormant genes.
Some bacteria develop enzymes that destroy the antibiotic molecule. For instance, beta-lactamase enzymes break apart the beta-lactam ring in penicillin, rendering it useless. Others modify the antibiotic’s target site so the drug can no longer bind effectively. Still others develop pumps that eject the antibiotic from the cell before it can do harm.
One of the most concerning forms of resistance is horizontal gene transfer. Bacteria can swap genes, even between different species, via plasmids—small circular pieces of DNA. A single plasmid can carry multiple resistance genes, arming a bacterium with defenses against several antibiotics at once.
Antibiotic resistance is not just a scientific curiosity—it is a looming crisis. Multidrug-resistant bacteria, such as MRSA (methicillin-resistant Staphylococcus aureus) and CRE (carbapenem-resistant Enterobacteriaceae), are increasingly common in hospitals. They are harder to treat, more expensive to manage, and often deadly.
Human Behavior and the Misuse of Antibiotics
Antibiotic resistance is accelerated by human actions. One of the most significant factors is the overuse and misuse of antibiotics. Doctors often prescribe antibiotics for viral infections, like the common cold, against which these drugs are useless. Patients may fail to complete a full course of antibiotics, leaving behind the hardiest bacteria to regroup and multiply.
In agriculture, antibiotics are used not only to treat sick animals but also to promote growth and prevent disease in crowded farming environments. This widespread use exposes bacteria to sub-lethal doses of antibiotics, creating ideal conditions for resistance to evolve.
The pharmaceutical pipeline for new antibiotics has slowed dramatically. Developing a new antibiotic is scientifically challenging, financially risky, and often unprofitable. As resistance increases, the need for stewardship and innovation has never been greater.
The Immune System and Antibiotics: A Crucial Alliance
Antibiotics do not fight bacteria alone—they work in concert with your immune system. While antibiotics weaken or kill bacteria, it is often your immune cells that clean up the remnants. Infections clear more quickly when both systems are working together.
In patients with compromised immune systems—such as those undergoing chemotherapy, transplant recipients, or people with AIDS—even minor infections can become life-threatening. Here, antibiotics act as a critical line of defense, stepping in for a weakened immune system.
But reliance on antibiotics alone is dangerous. We must preserve these drugs not only for ourselves but for future generations, especially those who may need them the most.
Strategies to Combat Antibiotic Resistance
Scientists and healthcare professionals are exploring multiple strategies to stay ahead in this microbial arms race. One approach is the development of new antibiotics that target previously untapped bacterial vulnerabilities. Some researchers are mining exotic environments—like ocean trenches or deep caves—for microbes that produce novel antibiotic compounds.
Another strategy involves modifying existing antibiotics to evade bacterial defenses. For instance, combining beta-lactam antibiotics with beta-lactamase inhibitors protects the drug from enzymatic destruction.
Phage therapy, an old idea given new life, uses viruses that infect and kill bacteria—bacteriophages—as precision weapons against resistant strains. Because phages are specific to their bacterial hosts, they can eliminate pathogens without disturbing beneficial microbes.
Vaccines can also reduce the need for antibiotics by preventing bacterial infections in the first place. Public health initiatives promoting hygiene, sanitation, and infection control help curb the spread of resistant organisms.
Most importantly, antibiotic stewardship—using antibiotics only when necessary and appropriate—remains our strongest defense.
The Future: A Fragile but Hopeful Outlook
We are at a crossroads. The miracle of antibiotics, once hailed as a medical triumph, is under threat from our own success. As bacteria continue to evolve, the urgency for innovation, education, and global cooperation grows.
New tools, such as artificial intelligence, are being used to predict resistance patterns and design drugs. Advances in genomics and synthetic biology may allow us to create tailor-made antibiotics or even probiotic treatments that outcompete harmful bacteria.
But technology alone will not save us. A shift in perspective is needed—recognizing that antibiotics are not unlimited, magic bullets, but precious and finite tools. Their effectiveness hinges not only on scientific progress but also on our behavior and responsibility.
Conclusion: Guardians of the Microscopic Frontier
The story of antibiotics is one of discovery, triumph, caution, and ongoing struggle. These molecules have saved countless lives, reshaped medicine, and altered the course of human history. They are the guardians of the microscopic frontier—protecting us from invisible foes that once held sway over life and death.
Yet the war is far from over. Every dose of antibiotics is a battle. Every prescription is a decision. Every resistant bacterium is a reminder that nature never sleeps.
As we move into an era where the effectiveness of antibiotics may dwindle, we must remember the lessons of the past, honor the tools we’ve been given, and forge new alliances between science, policy, and public awareness.
The battle between bacteria and medicine continues. Whether we emerge victorious depends on what we do next.